Juniper Publishers- Open Access Journal of Case
Studies
Polyostotic Fibrous Dysplasia: A Case Report
Authored by Vikram Khanna
Abstract
Introduction: Fibrous dysplasia is a relatively rare condition characterized by fibrous tissue replacement of the skeleton. It may implicate one or several bones and favors one side of the body. It begins in childhood and may progress beyond puberty and adulthood. Both sexes are equally affected.
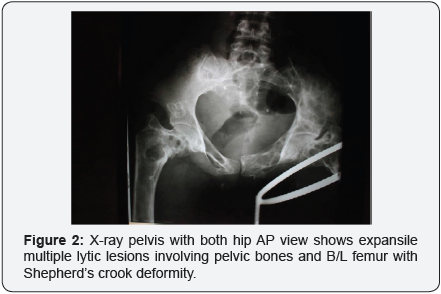
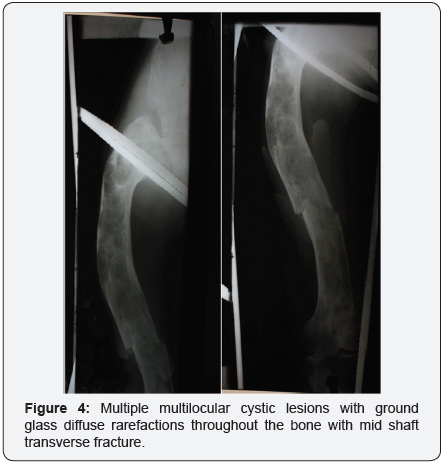
Case study: A 25 year old female presented with fracture in right femur after a trivial trauma. X-ray showed multiple multilocular cystic lesions with ground glass diffuse rarefactions throughout the bone with mid shaft transverse fracture. Similar lesions were seen in B/L Proximal humerus and Rt pelvis. Base of the skull showed Hyperostotic Bone formation. Bone Biopsy showed the mesenchymal stroma surrounding the dysplastic trabeculae is relatively hypocellular. There is a lack of osteoblastic rimming surrounding the dysplastic trabeculae. Both features are characteristic of fibrous dysplasia. The patient was managed with bisphosphonates and Thomas knee splint and union was seen in 2 months.
Keywords: Fibrous dysplasia; polyostotic; Ground glass; Shepherd crook deformity; GNAS1 gene
Introduction
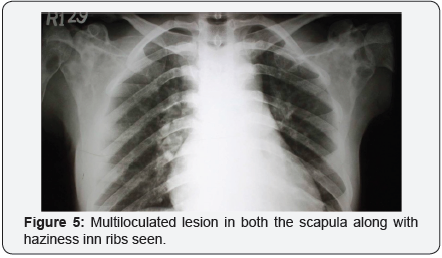
Fibrous dysplasia is a condition leading to abnormal differentiation of osteoblasts which leads to replacement of normal bone with fibrous stroma [1-3]. It may involve single bone (monostotic) or multiple bones (polyostotic). It may affect any bone however; skull and ribs are the commonest [2,4-6]. It is usually asymptomatic and is an incidental finding. It may become symptomatic when complicated by pathologic fracture or malignant change. It may be associated with aneurysmal bone cysts [6-12]. The mechanism of occurrence of ABC with Fibrous dysplasia is not known but it may be said that there may be a secondary disruption of osseous supply caused by the fibrous dysplasia leading to ABC. This association of ABC with fibrous dysplasia may lead to rapidly increase in growth which may be confused with malignant change [5,10]. We report a case of polyostotic Fibrous dysplasia in a 26-year-old lady showing the characteristic changes.
Case Report
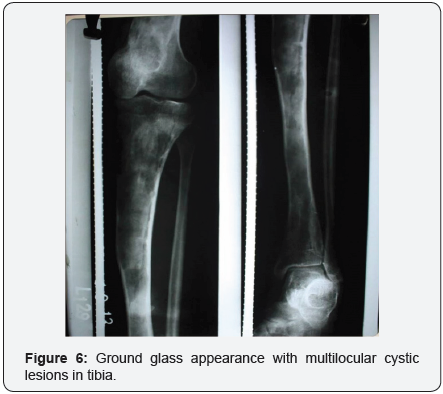
A 26 year old female presented with fracture mid shaft of left femur after having a trivial trauma. Patient had previous history of fracture in the right femur 4 years back presiding with limp and pain in right thigh.
On examination
- Anterior bowing of lt. thigh was seen.
- Swelling in the mid-thigh region 4×8cm
- Bony crepitus was present.
- Peripheral neurovascular status was normal.
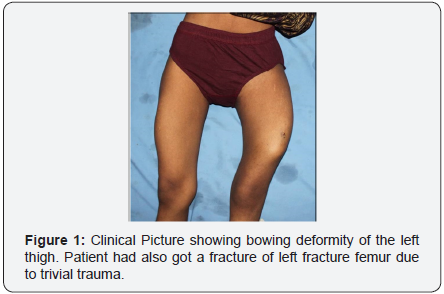
On x-ray
- Multiple multilocular cystic lesions with ground glass diffuse rarefactions throughout the bone with mid shaft transverse fracture.
- Similar lesions were seen in B/L Proximal humerus and Rt pelvis.
- Overlying cortex was thinned and expanded with thickened medial cortex with a typical ‘Shepard’s Crook Deformity’ due to varus deformity of the neck.
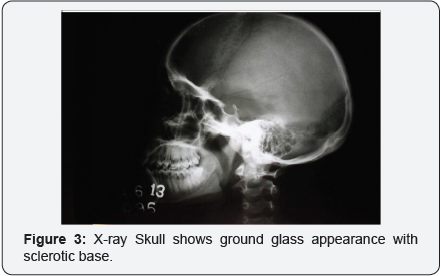
- Base of the skull showed Hyperostotic Bone formation.
Bone biopsy
I. The mesenchymal stroma surrounding the dysplastic trabeculae is relatively hypocellular. There was a lack of osteoblastic rimming surrounding the dysplastic trabeculae. Both features are characteristic of fibrous dysplasia.
II. A field of mature hyaline cartilage is shown adjacent to a bland fibrous stroma.
Lab reports
- Hb. = 9.6g/dl
- TLC = 9000 cells /ml
- DLC = n= 60 l=15 m=1 e=0 b=0
- Sr Ca =9mg/dl
- Sr alp = 60iu/l
- Sr phosphorus = 3mg/dl
- T3 = 160ng/dl
- T4 = 8 micro g/d
- TSH = 3 micro U/ml
Management
We treated our patient with zolindronic acid at time of presentation and at 3 months of the first injection. The patient was also kept on Thomas Knee splint for 2 months following which the fracture united and the patient was started with weight bearing ambulation.
Discussion
We treated our patient with zolindronic acid at time of presentation and at 3 months of the first injection. The patient was also kept on Thomas Knee splint for 2 months following which the fracture united and the patient was started with weight bearing ambulation.
The gross histological picture of fibrous dysplasia constitutes a firm solid grey-white mass which gradually replaces the medullary cavity and the surrounding cortical bone. This lesion is generally well circumscribed and well differentiated from the host bone. It consists of uniformly cellular fibrous tissue with a proliferation of bland and uniform spindle cells with sparse mitotic activity. Some nests of woven bones are also present without any significant osteoblastic rimming. Some bony spicules are also present in the curvilinear, “Chinese alphabet” pattern. Sometimes, the woven bone may be deposited in sclerotic, interconnected lamellae, cementoid bodies, or in orderly and parallel spicules [4,6,8,9,14].
X-rays features are not specific although they may be characteristic depending on the underlying histopathological picture. These features range from unilateral fusiform enlargement of medulla, deformity with cortical thickening, increased trabeculation to a characteristic “ground-glass” appearance which is formed by a mixture of immature bone and fibrous tissues [2,7]. On CT scan amorphous or irregular calcification may be seen. Magnetic resonance imaging maybe used in accurately defining full extent of the lesion.
Sudden increase in size of an existing fibrous dysplasia maybe due to superimposed ABC or malignant transformation [6,10,12,14]. Malignant transformation causes rapid increase in the size of the lesion but is rarely seen with an incidence of 0.5% in patients with monostotic FD. The incidence increases in patients with nearly 4% with McCune-Albright syndrome. It may develop after the involved bone getting irradiated. Most common malignant transformation is osteosarcoma followed by fibrosarcoma, chondrosarcoma and malignant fibrous histiocytoma [2,4,6,7,9,11,14]. Low grade osteosarcoma may mimic fibrous dysplasia. It maybe differentiated with the help of imaging and radiological features. Radiographic changes suggesting malignancy are lytic regions, intralesional calcification, periosteal reaction and a cortical disruption [6,9,14].
Histologically, malignancy like low grade osteosarcoma will include atypical mitotically more active cells than fibrous dysplasia. Also, the regularly spaced spicules which are seen in fibrous dysplasia will not be seen in osteosarcoma which shows malignant osteoid deposited in broader and irregular trabeculae [9].
Treatment of fibrous dysplasia for asymptomatic and stable lesions includes just monitoring of the patient. Surgery is only done for diagnostic biopsy, or to correct deformity, failure of non-surgical treatment prevention of pathological fractures and eradication of symptomatic patients. In polyostotic form bisphosphonate therapy may be used for the management and it leads to increase in the bone density and reduces the pain [3,4,7,13] (Figure 1-6).