Juniper Publishers- Open Access Journal of Case Studies
Dynamics of Frailty as a Geriatric Syndrome
Authored by Esra ATES BULUT*
Abstract
Frailty and sarcopenia are new geriatric syndromes which lead to poor outcomes including functional decline, falls, morbidity, hospitalization and mortality. Frailty is a distinctive health state related to the ageing process in which multiple body systems gradually lose their reservation capacity. It is a multidimensional state with interrelated factors in the physical, psychological, social, and environmental domains. It is also associated with other geriatric syndromes in the mood, cognition areas and physical performance. Clinically, diagnosis is based on weight loss, slow walking speed, low muscle strength and physical activity. Due to high frequency among seniors and being a reason of poor health outcomes, accurate diagnosis, and appropriate prevention and treatment strategies should be established.
Keywords: Ageing; Geriatric syndromes; Sarcopenia; Physical dependence
Introduction
Ageing process, frailty and death concepts belong to the mysterious subjects of medicine. Frailty is used currently different clinical meanings: easily broken, damaged, rapidly dying, diminished resistance and strength. It is a gradual process that develops slowly, and the rate of decline accelerates with acute events. Once a person becomes frail, a progressive process proceeds until death [1]. Many health care providers focus on diseases when they evaluate patients. However, frailty does not fit to this approach, and it is not the chief complaint. Patients are usually asymptomatic, or the findings are subtle [2]. Frailty is defined difficulty in restoring the homeostatic balance against stressors with ageing. Frailty has multidimensional state with interrelated factors in the physical, psychological, social, and environmental domains that affect the physiologic reserve of the systems. Furthermore, it is also indicated as a geriatric syndrome characterized by reduced physical function, which may lead to decreased strength, endurance, and increased dependence or mortality [3]. Because of the reduced capacity of the organism, the risk of developing poor health outcomes such as falls, hospitalization, disability, discharge to nursing home and mortality increases [4,5].
Although ageing is considered as frailty in society, every elder is not frail. Prevalence of frailty in subjects aged 65-75 years ranges from 3% to 7% [6]. This rate rises to 32% over the age of 90 years [7]. The prevalence of frailty differs from various ethnic groups and increases with age.
Frailty can be primary or secondary diagnosis. 7% of frail older adults do not have a systemic disease. Moreover, 25% have only one disease [8]. However, an acute event, atherosclerosis, infection, malignancy, depression or the last period of a chronic process may cause frailty. It has been reported increased age, history of cancer, chronic obstructive pulmonary disease, cerebrovascular disease, physiological impairments of inflammatory processes and coagulation are risk factors for frailty [9].
Discussion
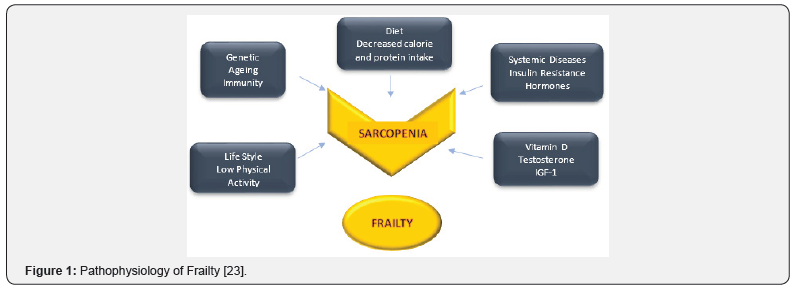
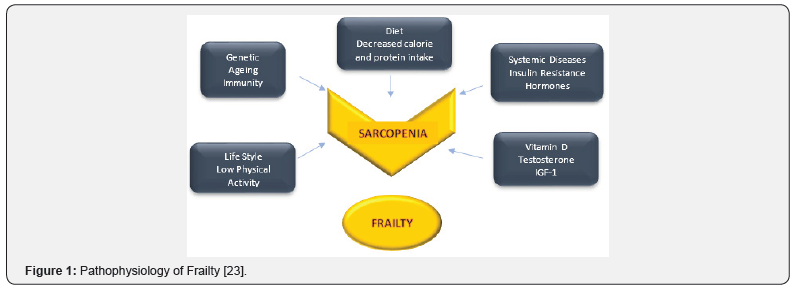
Pathophysiology
Frailty characteristics are associated with overt changes in the four main title: body composition, homoeostatic dysregulation, energetic failure and neurodegeneration. In addition, impaired glucose metabolism, inflammatory biomarkers, and some physiological variables such as markers in clotting pathway contribute the pathophysiologic pathway [7]. Many physiological systems including the central nervous system, the sympathetic nervous system, the endocrine system, the skeletal-muscular system and the immune system are affected. Which system is affected first and what threshold level is needed to develop the clinical situation are the key questions to be answered at the moment.
Age-related skeletal muscle loss or sarcopenia is the main feature of frailty. Preservation of skeletal muscle function requires the interaction of many factors, such as hormones, neurological functions, inflammatory markers, and nutrients [10]. Recent studies showed infiltration of the muscle by fat tissue causes decrease in the muscle strength and mass. It was reported adipose tissue especially visceral fat tissue, can cause some hormonal and inflammatory changes which contribute release of inflammatory cytokines and hormones [7]. Interleukin-6 (IL-6), Tumor Necrosis Factor-α (TNF-α) and other inflammatory mediators cause muscle destruction for energy production [11]. Increasing evidence indicates these markers may cause skeletal muscle loss by inducing apoptotic mechanisms [12]. As a result, metabolically active fat stores establish chronic inflammatory state and increase sarcopenia. Many studies have shown inflammatory markers such as IL-6, CRP, white cells, and macrophage counts are related to frailty [13]. These findings suggest that chronic, low level of inflammatory activity induce frailty. Increased IL-6 causes reduction in bone mineral density, muscle loss, anemia, insulin resistance, hypothalamo-pitiuter-adrenal axis stimulation and impaired immune system regulation [14]. Recent studies reported hyperinsulinemia and hypertriglyceridemia lead to suppression of appetite and nutritional intake. Besides, they may also be associated with cognitive impairment, physical decline and leptin resistance [15].
It was hypothesized cognitive impairment, physical inactivity, visual-hearing loss and incontinence were related to frailty in women [16]. The coexistence of cognitive and physical impairment may be explained by the role of proinflammatory cytokines in the pathophysiology of both conditions [17].
Three main hormones decrease with ageing: growth hormone, sex steroids and adrenocorticoid hormones [18]. Sex steroids and growth hormone affect age-related changes in body composition. IGF-1 plays major role in the development of skeletal muscle cells, however inflammatory cytokines suppress IGF-1 release [19]. Furthermore, dehydroepiandrostenodion sulfate (DHEAS) suppresses inflammation induced by nuclear factor kappa B. Reduced DHEAS and testosterone levels were thought to related to frailty [20,21]. In addition, impaired cortisol diurnal rhythm is associated with increased catabolism, muscle loss, anorexia, and decreased energy expenditure, which are the main building blocks of frailty [22]. Changes in cellular ageing pathways, disruption of telomeric structures, mitochondrial dysfunction, increased free radical production, decreased DNA repair capacity with ageing may explain reduction of multisystem physiological regeneration capacity. Figure 1 summarizes pathophysiology of frailty [23].
Diagnosis
Because of the increase the number of older adults who need medical support, and cost of these patients to the healthcare system, it has great importance to determine the biological older patients. In the last two decades, it is desirable to develop biomarkers and scales to distinguish the biological age of older individuals [24]. Therefore, patients should be evaluated not only disease-oriented but also function-oriented.
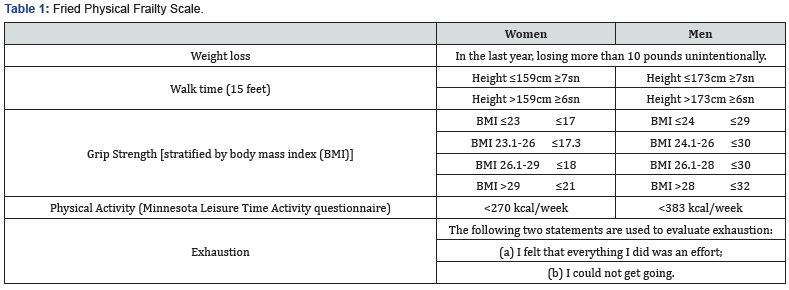
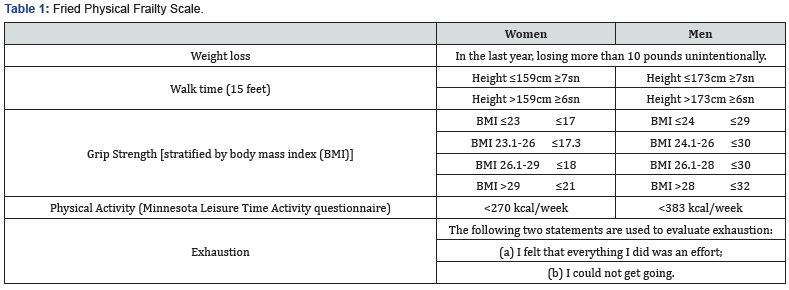
Fried and his colleagues composed the most frequently used criterion to assess vulnerability. The Fried Physical Frailty Scale is shown in Table 1 [25]. Frailty is defined in this phenotype model as presence of 3 or more of the following: exhaustion, weight loss, low muscle strength, low walking speed, and of low physical activity. The presence of one or two criteria was considered as pre-fail state. The walking speed, muscle strength and physical activity are evaluated by 4-meter walking test, hand grip test (dynamometer) and Minesota Leisure Time Activity questionnaire, respectively. This model successfully predicts poor health outcomes such as falls, disability, hospitalization, and mortality [25].
Due to the difficulty of application the phenotype model in daily clinical practice, various other scales were developed. The FRAIL scale has 5 criteria: fatigue, resistance, ambulation, systemic diseases (ilness) and weight loss [26]. Presence of 1-2 criteria is considered as pre-frail state and 3 or more criteria indicates frailty
The cumulative deficit model was then established by the Canadian Health and Ageing Study. Total 92 basal variables were included in this study, including various findings (e.g. tremor), symptoms (e.g. low mood), disease states, abnormal laboratory values, and disabilities. Vulnerability was assessed by the accumulation of deficiencies in patients. The more deficiencies patients have, the worse frailty status they have [27]. In addition to these scales, other indexes with wider psychosocial contents such as the Groningen and Tilburg Frailty Indicators were also developed [28,29].
A meta-analysis which was conducted between 2009-2015, assessed 29 frailty scales, according to this meta-analysis [30], the Fried physical scale and the deficit index are the most commonly used scales. Fried phenotype model, frailty deficit index, Edmonton frailty scale and clinical frailty scale were found both reliable and well predict clinical results.
Prevention and treatment
Because frailty is more common with increasing age, it is important to apply protective approaches from middle ages. Early recognition and effective treatment strategies have great importance in order to prevent frailty in later life.
Optimal treatment of patients’ systemic medical diseases and stable management of intervening acute conditions constitute the basic principles of frailty treatment [31]. Currently, there is strong evidence that exercise is more beneficial than other interventions in frail patients. Multi-component exercises such as resistance, flexibility, aerobic and balance exercises are useful in the prevention and treatment of frailty. In addition, it is also considered to be the best strategy to prevent the development of disability in the frail patients [32,33]. However, the most effective type, duration and frequency of exercise intervention is uncertain.
Vitamin D support is known to reduce falls, hip fracture and mortality in older adults [34-36]. Vitamin D is also effective on neuromuscular functions [37]. Although, there are no large scale studies, replacement of vitamin D deficiency seems to be effective for the treatment of frailty.
In 2013, consensus for frailty was determined treatment of physical frailty under 4 main headings: [3]
a) Exercise
b) Calorie and protein supplement
c) Vitamin D
d) Prevention of polypharmacy
Conclusion
Prevention of frailty should not only be considered as a necessary intervention for the elderly. Effective prevention of systemic diseases starts at early ages. Promoting healthy lifestyle and improving health services should be considered as main targets for successful ageing. However, primary care practitioners should be aware of frailty and risky individuals should be referred to necessary higher levels of health care service. Furthermore, clinicians should keep frailty on mind in individuals over 70 years with unintentional weight loss. Recognition of frailty identify high risk patients for medical interventions and reduce risk of adverse outcomes. In the future, universal, valid diagnostic criteria should be established, and more detailed studies are needed to clarify the pathophysiology of frailty.
For more articles in Juniper Publishers | Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment