Juniper Publishers- Open Access Journal of Case Studies
Morbidity, Mortality and Major Bile Duct Injury in 2296 Patients Undergoing Laparoscopic Cholecystectomy - Review of Literature
Authored by Shing-Moo Huang
Abstract
Aims: The aims were at the safety of laparoscopic cholecystectomy in the treatment of gallbladder diseases in a series of 2296 patients. Also reports in literature were reviewed.
Materials: Between January 1, 1999 and July 31, 2013, 2296 patients with gallbladder disease undergoing laparoscopic cholecystectomy were recruited. Demographics such as age, gender, indications, associated diseases, conversions, stone types, perioperative morbidity, major bile duct injury and mortality were recorded.
Results: There were 61 conversions. The conversion rate was 2.7%. Indications for laparoscopic cholecystectomy include symptomatic gallstones (2,135, 93%), gallbladder polyps (115, 5%) and others (46, 2%). We found our morbidity rate was 2.18% (50), mortality rate 0.04% (1) and major bile duct injury rate 0.08 (2).
Conclusion: In this observational study, it was found the morbidity, mortality and major bile duct injury rates were lower than those of laparoscopic cholecystectomy reported. The mortality and major bile duct injury rates were also lower than those of open cholecystectomy reported. However morbidity rate of our series was higher than that of open cholecystectomy.
Keywords: Laparoscopic cholecystectomy; Morbidity; Mortality; Safety: major bile duct injury
Introduction
Phillippe Mouret performed the first videoscopic laparoscopic cholecystectomy on a human patient in 1987 [1]. Since then, this new advancement in the history of general surgery has gained wide acceptance and entered daily practice for general surgeons throughout the world [2-8]. With a few exceptional randomized controlled studies [6], most efficacy and safety studies for laparoscopic cholecystectomy were observational and retrospective case controlled studies [9]. Therefore, this study aims at the safety of laparoscopic cholecystectomy as compared among those of reports in the literature and the author’s personal series. Safety of open cholecystectomy was also compared.
Materials and Methods
Patients
This is an observational study. Between January 1, 1999 and July 31, 2013, 2296 patients with gallbladder disease were recruited and underwent laparoscopic cholecystectomy by the author at Veterans General Hospital–Taipei and Chung Shan Medical University.
Results
Demographics
The M/F ratio was 1:1.03 for symptomatic gallstones, 1.661:1 for chronic cholecystitis but 1.25:1 for acute and sub-acute cholecystitis. In acute cholecystitis patients, male predominant was found whereas female predominant was found in chronic cholecystitis patients (P < 0.0001). The average age for patients with symptomatic gallstones, chronic cholecystitis and acute cholecystitis are 54±15, 53±15 and 57±17 years old.
Indications for laparoscopic cholecystectomy
These include symptomatic gallstones (2,135, 93%), gallbladder polyps (115, 5%) and others (46, 2%).
Morbidity and mortality
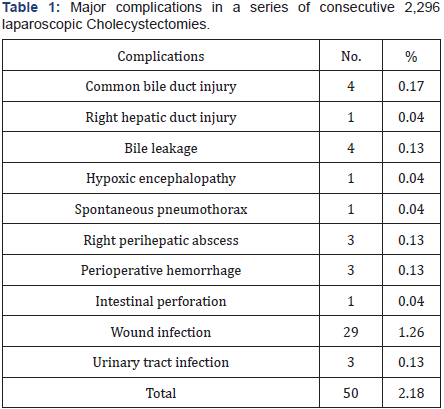
There are 50 operative complications (50/2,296, 2.18%), i.e., common bile duct injury (4, 0.17%), right hepatic duct injury (1, 0.04%), bile leakage (4, 0.17%), hypoxic encephalopathy (1, 0.04%), spontaneous pneumothorax (1, 0.04%), right perihepatic abscess (3, 0.13%), perioperative hemorrhage (3, 0.13%), intestinal perforation (1, 0.04%), wound infection (29, 1.26%) and urinary tract infection (3, 0.13%) (Table 1).
The patient complicated with hypoxic encephalopathy was a 76-year-old male diagnosed with gallstone with acute cholecystitis. Preoperative electrocardiogram did not reveal any cardiac arrhythmia. The operative procedure was uneventful except that it was a relatively long procedure. The operation time was 121 minutes. An episode of bradycardia developed which was followed by a cardiac arrest.
After resuscitation, the patient’s heartbeat and respiration returned. However, the consciousness did not return. Glasgow coma scale was 4 (E1V1M2). The patient did not recover from the hypoxic encephalopathy and finally succumbed to consequent pneumonia. This is the only mortality in this series. The patient complicated with spontaneous pneumothorax was a 65-year-old male associated with chronic obstructive pulmonary disease. Intra-operatively, the anesthesiologist noted a drop of oxygen saturation from 98% to 90% at 50% alveolar oxygen concentration. Auscultation revealed decreased breathing sound over right lung field. Emergent insertion of a pigtail drain into right pleural cavity revealed a jet of air emitting out. The operation was completed smoothly. The pigtail was removed 3 days postoperatively and was discharged on 4th postoperative day.
There were 32 surgical infections associated with laparoscopic cholecystectomy in this series (1.39%), including 3 (0.13%) right peri-hepatic abscesses and 29 (1.26%) wound abscesses. The former tended to suffer from spiking fever and right upper abdominal pain 2 weeks after laparoscopic cholecystectomy. Ultrasonography revealed sonolucent fluid collections around peri-hepatic spaces were detected. Ultrasound-guided insertion of pigtail drains and intravenous antibiotics were all that were needed to resolve these conditions. The patients were discharged around 7 days later. The latter were managed by incisional drainage and open wound dressings successfully.
There was one patient who had undergone previous abdominal surgery. This 56-year-old male patient underwent laparoscopic cholecystectomy for gallbladder stone with open laparoscopic technique. A severe small intestinal loop adhesion directly under the umbilicus was found. The procedure was completely. However, on the 3rd postoperative day, profuse yellowish small intestinal contents flew out from the infraumbilicus trocar wound. The patient underwent immediate reoperation and a 6 cm transverse extension of the infra-umbilicus wound was performed. A small 0.3 cm perforation hole was found at a mid-jejunum loop located immediately below the umbilicus. Primary repair with peritoneal cavity lavage was performed and the wound was closed. The postoperative course was uneventful and the patient was discharged 7 days later.
Three patients suffered from urinary tract infections. They received Foley catheter insertion after general anesthesia because longer operation was expected. Among them, two were from the contracted gallbladder group. Antibiotics and sulfa drugs were all that were needed to resolve the condition (Table 1).
Biliary complication
There were 2 patients with major bile duct injury (patients 1 and 8 in Table 2), 3 patients with minor bile duct injury (patients 5, 6 and 7) and 4 patients’ with delayed bile leakage (patients 2, 3, 4 and 9, Table 2).
Major bile duct injury patients required more sophisticated repairing procedures, such as hepato-jejunostomy or choledochojejunostomy (patient 1 and patient 8). Their prognosis needs longer periods of follow-up to make sure they are not inflicted with recurrent cholangitis like biliary cripples, as patients 1 and 8 were devoid of these episodes for 6 - 7 years.
Minor bile duct injury patients required only simpler managements, such as, primary repair with T-tube splinting or simple T-tube insertion would suffice in patients 5, 6 and 7. The prognosis was usually good.
Patients with delayed bile leakage also required only simple management, such as, T-tube insertion, which solved the problem in patients 2, 3, 4 and 9. Their prognosis was uniformly good within 7 days (Table 2).
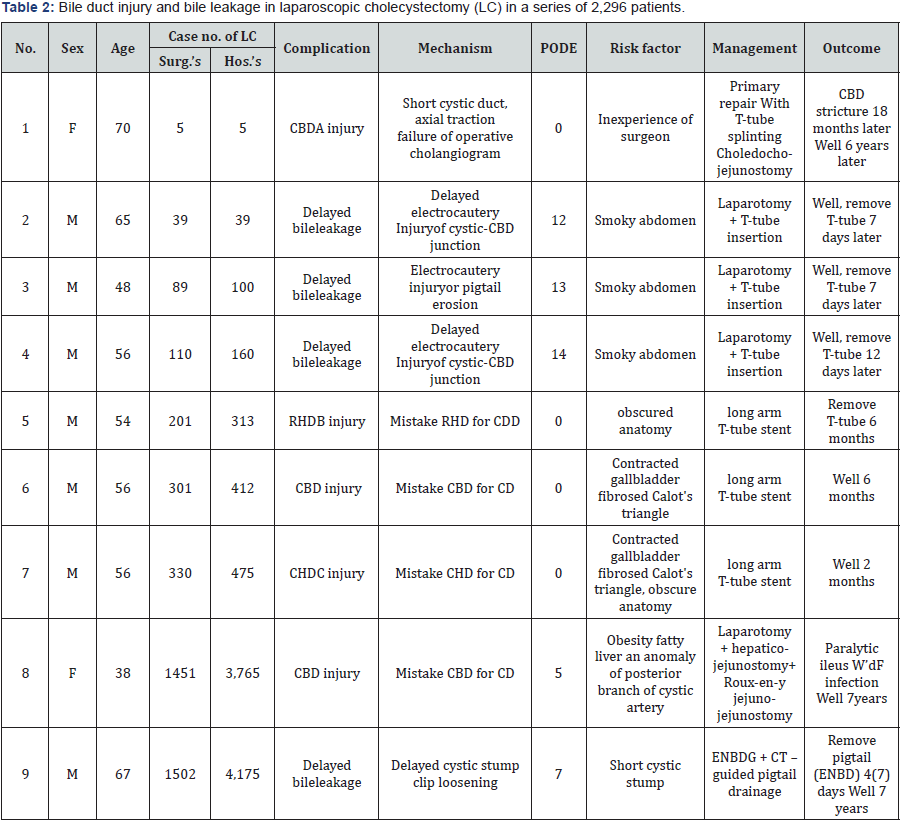
ACBD: common bile duct, BRHD: right hepatic duct, CCHD: common hepatic duct, DCD: cystic duct, E: POD: post-operative day, FW’d: wound, GENBD: endoscopic naso-biliary drainage.
Discussion
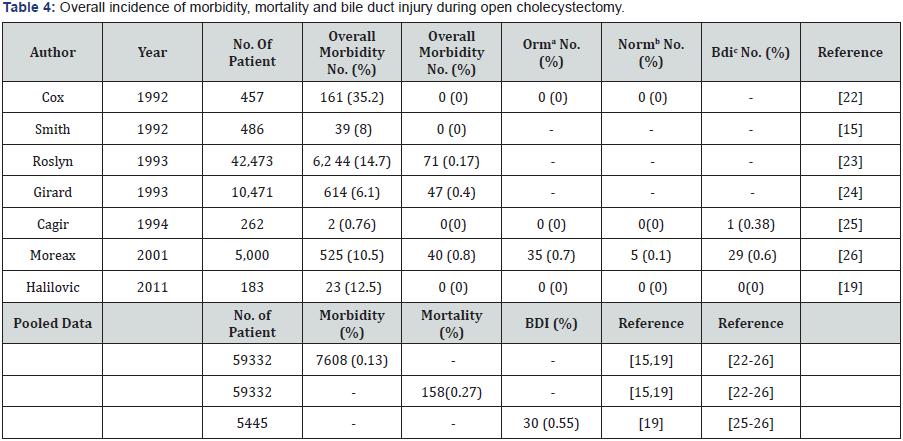
Undoubtedly, laparoscopic cholecystectomy is the greatest arena for laparoscopic surgery. From literature, the overall morbidity and mortality of laparoscopic cholecystectomy are no different from those of open cholecystectomy. From Tables 3 & 4, the average morbidity of laparoscopic cholecystectomy is 5.2% (range 1.2% - 23.3%) whereas that of open cholecystectomy is 0.13% (range 0.76% - 35.2%). The average mortality of laparoscopic cholecystectomy is 0.46% (range 0%-0.8%). The average mortality of open cholecystectomy is 0.27% (range 0.0% - 0.8%). There is a pattern of the incidence of major bile duct injury requiring biliary reconstruction corresponding to the case number of the surgeon. Major bile duct injury is high or none in the surgeon’s learning curve period (the first 100 cases to less than 500 cases, Table 3), also as in case 1 of Table 2 in this series. Not with standing the experienced surgeon has past the learning curve period, the incidence of major bile duct injury did not fall [10,11]. It looks as if when surgeon passed his first 500 and less than 1,000 cases, he begins handling more complicated cases and major bile duct injury incidence tends to re-appear, i.e., 0.79-1.4%, as case 9 of Table 2 in this series. With further experiences gained with increasing case number beyond 1,000 the surgeon’s laparoscopic cholecystectomy-associated incidence begins to descend and level off, i.e., 0.1-0.6% [8,12- 13].
In this observational study of 2,296 patients undergoing laparoscopic cholecystectomy, we found our morbidity rate was 2.18% (50/2,296), mortality rate 0.04% (1/2,296) and major bile duct injury rate 0.08 (2/2,296), lower than the average of those of laparoscopic cholecystectomy in the literature: 5.2% (8,072/155,622, Table 3), 0.46% (27,635/6,040,632, Table 3) and 0.22% (16,382/7,559,461, Table 3). In mortality rate and major bile duct injury rate, we found our series are lower than the average of open cholecystectomy in the literature: 0.04% (1/2,296) and 0.08 (2/2,296) vs. 0.27% (158/59,332, Table 4) and 0.55% (30/5,445, Table 4). However, in morbidity rate, our series are higher than the average of open cholecystectomy in the literature: 2.18% (50/2,296) vs. 0.13% (7,608/59,332, Table 4).
In turn, for morbidity rate, the order of lowest rate was: the average of open cholecystectomy in the literature 0.13% (7,608/59,332, Table 4), our series 2.18% (50/2,296) and then laparoscopic cholecystectomy in the literature5.2% (8,072/155,622, Table 3). For mortality rate, the order of lowest rate was: our series 0.04% (1/2,296), the average of open cholecystectomy in the literature 0.27% (158/59,332, Table 4) and then the average of laparoscopic cholecystectomy in the literature 0.46% (27,635/6,040,632, Table 3). For major bile duct injury rate, the order of lowest rate was: our series 0.08 (2/2,296), the average of laparoscopic cholecystectomy in the literature0.22% (16,382/7,559,461, Table 3) and then the average of open cholecystectomy in the literature of open cholecystectomy 0.55% (30/5,445, Table 4).
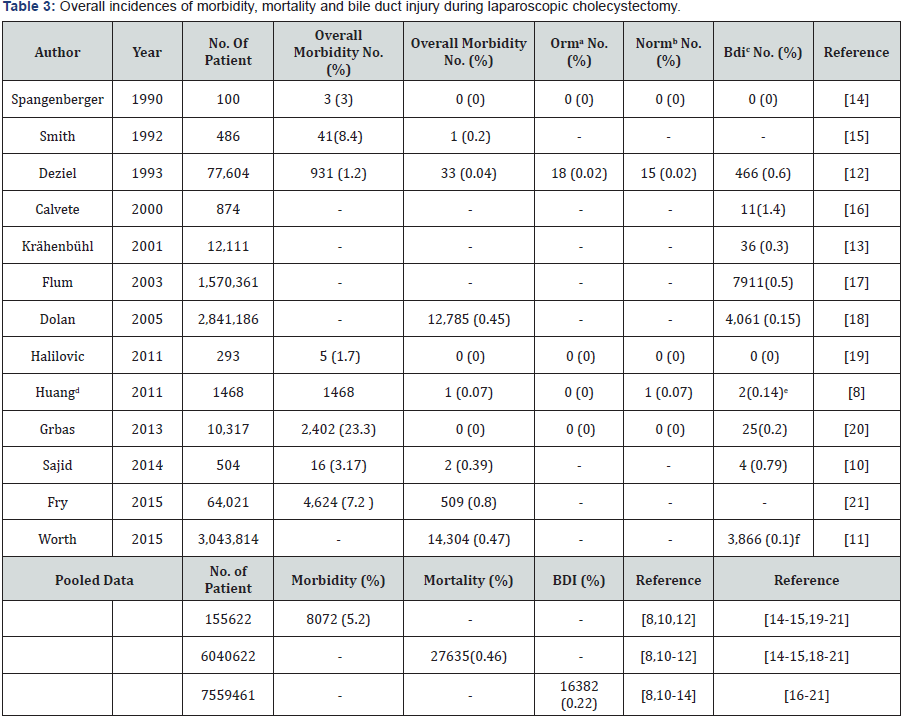
aoperation related mortality bnon-operation related mortality cmajor bile duct injury.
Conclusion
In conclusion, an observational study was conducted on 2296 patients with gallbladder disease undergoing laparoscopic cholecystectomy. It was found our morbidity, mortality and major bile duct injury rates were lower than those of laparoscopic cholecystectomy reported in the literature. The mortality and major bile duct injury rates were also lower than those of open cholecystectomy reported in the literature. However morbidity rate of our series was higher than that of open cholecystectomy.
For more Open Access Journals in JuniperPublishers please click on:
https://www.linkedin.com/company/juniper-publishers
For more articles in Open Access Journal of Case Studies please
click on: https://juniperpublishers.com/jojcs/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jojcs/JOJCS.MS.ID.555620.php


