Happy New Year from Juniper Publishers!!!
Pandemic year 2020 has shown us what we can bear, may this coming year remove all this negative energy and enlighten our lives Happy New Year!!!
Juniper Publishers Journal of Case Studies is an international, peer reviewed open access journal, focussed on bringing out premium quality case reports in all areas of basic medical sciences and clinical specialities. ‘JOJCS’ aims to serve as a repository of medical case reports that can go a long way in enriching the professional knowledge of medical practitioners around the world.
Happy New Year from Juniper Publishers!!!
Juniper Publishers- Open Access Journal of Case Studies
Dirofilaria is a filarial nematode that causes natural infection in mammals like dogs, felids, foxes, beavers etc. and humans are accidental hosts. We report here a case of Dirofilaria recovered from the subconjunctival tissue of the eye of a 55yrs old male patient, who presented with complaint of swelling in his right eye.
Keywords: Dirofilaria; Subconjunctival; Human
Dirofilaria is a filarial nematode that causes natural infection in mammals like dogs, felids, foxes, beavers etc. Humans are accidental hosts and out of forty species of Dirofilaria identified, D. repens and D. immitis have been most commonly associated with human infections [1-3]. All Dirofilaria larvae are filariforms. The infecting larva is the filariform larva of third stage or L3. Culicid mosquitoes belonging to any of these genera; Anopheles, Culex, Aedes, Mansonia, Culiseta and Armigeres can act as the vector for the transmission of the infection. The L3 larvae penetrates the human tissue usually don't survive and those that manage to survive may develop into adult worms but they cannot fully develop in humans and do not produce microfilariae as a general rule [4]. There are exceptions to this rule in literature where adult worms in human tissue can also produce microfilaria [4-6].
D. immitis is a parasite that commonly infects cardiovascular system of canines and also has the potential to involve human pulmonary system. D.repens commonly localizes in the subcutaneous tissue of definitive host and in humans infection usually presents as solitary nodule but the worm may migrate in the subcutaneous tissue causing creeping eruptions and rarely may it infect other organs like lungs, female breast or eye. Ocular involvement may be orbital, periorbital, sub-conjunctival or intra-vitreal [7,8].
We report here a case of Dirofilaria recovered from the subconjunctival tissue of the eye of a 55 years old male patient, who was presented with complaint of swelling in his right eye.
A 55-year-old male reported to ophthalmology OPD in a tertiary care centre, New Delhi with complaint of pain and redness in the right eye since 5 days. On examination, a tender sub-conjunctival cystic swelling of 1x1cm was detected under the bulbar conjunctiva on the temporal side of the right eye with congestion. Visual acuity was 6/6 in both the eyes and other ocular examination was within normal limits. There was no history of injury, allergy or any previous lesions in the eye.
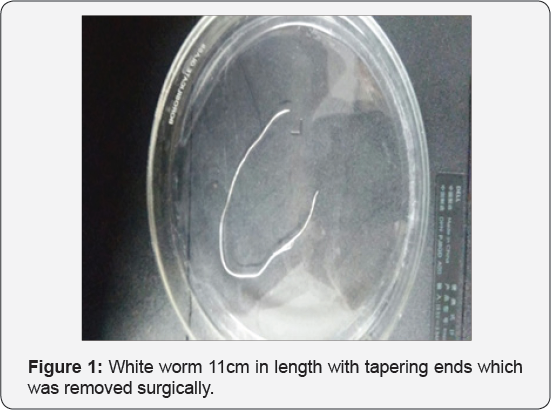
The patient was non-hypertensive, non-diabetic with no other systemic illness. There was no history of travel to other places in the last two years. An examination of the patient's stool did not reveal any parasitic ova or cyst and peripheral blood smear did not show eosinophilia or microfilaria. A surgical procedure was undertaken to remove the cyst and during the procedure a live coiled worm was seen moving in the cyst which was gently extracted with a pair of forceps. The worm was referred to the Department of Microbiology in formal saline for establishing its identification. The worm was identified using morphological features published by Levine [9]. The worm was white, elongated, 0.5mm thick and 11cm in length while at the two ends it was comparatively thin (Figure 1). The cuticle was multilayered with distinct longitudinal ridging (Figure 2) and the anterior end of the worm was showing mouth and the esophagus tube with a vulval opening. Based on the size, cuticular and internal morphologic features, the worm was resembling adult female Dirofilaria (Nochtiella] repens. No further treatment was required after removal of worm (Figure 3).


Dirofilariasis is a zoonotic infection that was once considered endemic to Mediterranean countries, is being reported from different corners of the world including Africa, Australia, America and Asia. Six of the forty reported species of the Dirofilaria; D. immitis, D. repens, D. striata, D. tenuis, D. ursi and D. spectans are known to cause disease in humans [1]. D. immitis is responsible for pulmonary Dirofilariasis, while D. repens has been associated with subcutaneous and ocular pathologies [10].
Since the publication of first report of D. repens by Angelo Pace in 1867 [11], there has been gradual increase in the number of cases, with majority of them reported in the last couple of decades itself. Pampiglione et al. [3] document reference of 782 cases caused by D. repens worldwide with 372 of them reported only from 1995-2000 [3]. With another fifteen years into this century, this figure is likely to have multiplied further
In India, Dirofilariasis is considered endemic to Southern states of India and the first recorded report of human ocular Dirofilariasis is from Kerala in 1976 [12]. However cases have also been reported from northern and western regions of the country [13]. Patel et al. [14] in their brief communication of 2014, document reference of 19 cases of human Dirofilariasis from India as on 15th July 2011 [15]. This figure is expected to increase further with fresh reports. Most of the documented cases of human Dirofilariasis recorded in India had ocular infections, with few case reports showing subcutaneous Dirofilariasis [12,13].
Clinical features of ocular Dirofilariasis depend upon the actual site of ocular area affected; skin of eyelid, conjunctiva, the tenon membrane, a retrobulbar space or intrabulbar structures. The site of localization of the parasite has direct bearing on the associated disability and complications. The most common localization is sub-conjunctiva or sub-tenon space and the diagnosis in both the situations is easier and more exact because the conjunctiva is transparent and possibility of direct detection of parasite is significant. In this particular case, the lesion was in the form of a cyst and a simple incision into the cyst made the worm wriggle out of the lesion. The worm was identified as D. repens on the basis of morphological features.
Direct examination of the parasite remains the mainstay of diagnosis because the robust serological systems are not available and eosinophilia that may be detectable in about 15% cases usually doesn't help steering the course of narrowing down the differential diagnosis [16]. Presently, no diagnostic system for early diagnosis of this infection is available and the necessity of this modality appears essential to avoid unnecessary investigative trauma on grounds of misdiagnosis of the condition as malignant tumour.
Removal of the parasite through surgical intervention or conventional extraction methods is the treatment of choice. Since there is no microfilariaemia, the antihelminths may have no therapeutic role and the use of antifilarial drugs is not evidenced in literature, though prophylactic use of DEC [Di Ethyl Carbamazine] or Ivermectin may be considered to destroy any worm that may be occupying some cryptic location and may not be producing any clinical trouble [13, 17]. Moreover, human Dirofilaria infection with more than one worm is rare and infrequent.
Human Dirofilariasis could be an emerging zoonotic infection though there appears to be underreporting of cases on account of cases remaining undiagnosed or unpublished. With roaring population of dogs and cats combined with teeming numbers of mosquito vectors, this infection appears to have all the epidemiological instruments available to establish itself firmly in northern India and Dirofilariasis once considered endemic to southern India can make its pan India presence visible very emphatically. There is need to raise awareness among the medical scientists to the issues and challenges related to diagnosis and management of human Dirofilariasis. Also, preventive strategies like; chemoprophylaxis of animals and vector control, require to be put in place since the parasite involving cardiovascular system has the potential to cause significant morbidity.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
Juniper Publishers- Open Access Journal of Case Studies
Central Nervous System complications of retroviral infection are common. The patho-physiology of many of these complications is still not well understood. In 10-20% of symptomatic retroviral infections, neurological disease is mostly the primary manifestation of AIDS. Intracerebral hemorrhages seem to be less frequent than cerebral ischemia in retropositive patients, and are often associated with thrombocytopenia, aneurismal or primary CNS lymphoma.
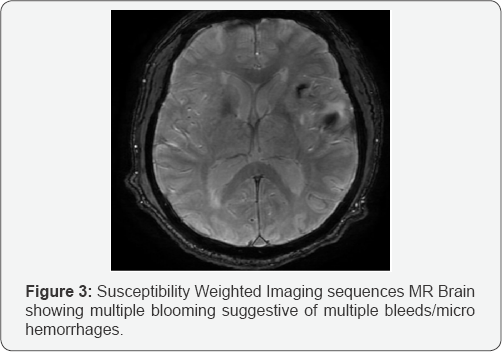
We report a case of multiple unilobar bleeds in retroviral disease patient, the etiology of which is not attributable to the above mentioned causes. We postulate that having ruled out the above mentioned possibilities, HIV associated vasculopathy (HAV) may be the most likely cause of such multiple intracranial bleeds in patients with retroviral disease. To the best of our knowledge, it has been rarely reported in the past. While investigating such bleeds, Susceptibility Weighted Imaging (SWI) MRI is a useful technique to determine additional old hemorrhages (due to hemosiderin deposition). We recommend that Digital Substraction Angiography (DSA) should be done in all such cases, to rule out other cause of bleed such as arteriovenous malformation, aneurysm, Primary CNS Lymphoma.
Keywords: Multiple unilobar intracranial bleeds in HIV; Intra-cerebral bleed in HIV
Abbreviations: CNS: Central Nervous System; HIV: Human Immunodeficiency Virus; AIDS: Acquired Immuno Deficiency Syndrome; HAV: HIV associated vasculopathy; DSA: Digital Subtraction Angiography; UMN: Upper Motor Neuron; BP: Blood Pressure; mmHg: millimeters of mercury; Aptt: Activated partial thromboplastin time; PT: Prothrombin Time; INR: International Normalized Ratio; RVD: Retro Viral Disease, ANA: Anti Nuclear Anibodies ; ANCA: Anti Nuclear Cytoplasmic Antibodies
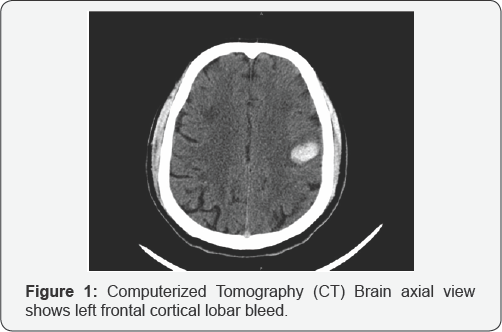
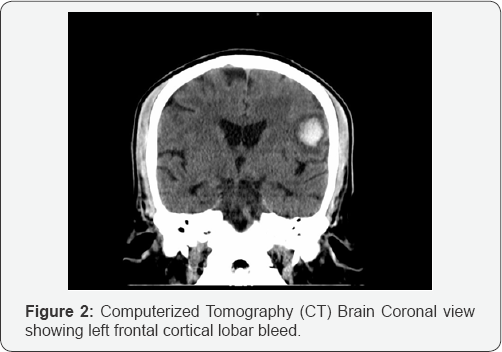
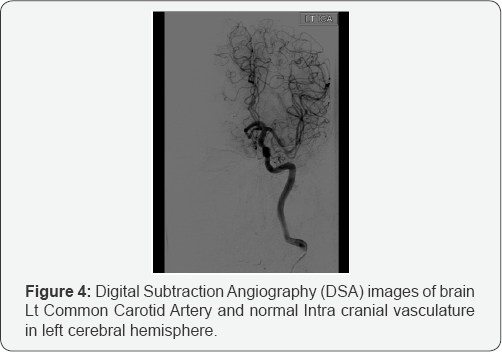
A 55 year male known case of Retroviral disease (RVD) positive illness, on Antiretroviral medications (Zidovudine, Lamivudine and Nevirapine) presented with abrupt onset difficulty in speaking, deviation in angle of mouth to left. On examination, was found to have motor aphasia (non-fluent), impaired repetition, though comprehension was normal. Right Upper Motor Neuron (UMN) facial palsy, brisk Deep tendon reflexes (DTR) on right side with ipsilateral plantar extensor. CT Brain showed Left Frontal lobar hematoma (Figure 1 & 2). MRI Brain showed left frontal bleed with multiple chronic micro bleeds (Figure 3). Digital Subtraction Angiography [DSA] was normal (Figure 4 & 5), ruling out any arterio-venous malformations or aneurysms. The patient was not a known case of hypertension. All his blood pressure reading post admission were normal prior to this event. The blood pressure (BP) recorded soon after the onset of neurological deficits was 170/100mmHg. HIV 1 was confirmed with western blot test, CD 4 count 940, other lab reports normal. Coagulation profile activated prothrombin time (PTT), prothrombin Time (PT), International Normalized Ratio (INR), platelet count were normal. The other investigations included cardiovascular workup (electrocardiogram and echocardiography), chest x ray, bilateral carotid artery Doppler of extra cranial neck vessels, ultrasonography of abdomen and pelvis , CSF analysis and culture.
Blood investigations such as Anti-NuclearAntibodies (ANA), Anti-Nuclear Cytoplasmic Antibodies (ANCA), serological testing for syphilis fasting serum lipids, random blood sugars, fasting and post prandial blood sugars, serum electrolytes, renal function tests (creatinine, urea) and full blood count. Renal artery Doppler done as a work up for newly detected hypertension. All the above mentioned investigations were normal.
Differential Diagnosis considered were: Aneurysmal bleed; AV Malformation; Primary CNS Lymphoma. Patient was treated with antihypertensive, antiretroviral and speech therapy. The patient gradually improved partially and had improving motor aphasia at the time of discharge.
ICH is a less common but known entity in young stroke in HIV and non-HIV patients. The common causes for intracerebral lobar bleeds are arterio-venous malformations, cavernomas, aneurysms, tumors like primary CNS Lymphoma, which bleed. Once these causes are ruled out, the other common cause of such lobar bleeds in HIV associated vasculopathy (HAV) [1].
HIV-induced amyloid deposition in cerebral vessels causing vasculopathy is a known cause of Intra cerebral bleed in HIV patients. Some evidence to that effect is found on multiple post autopsy histopathological studies, which have shown perivascular amyloid deposits in young HIV-positive individuals. Amyloid deposition in cerebral vessels increases the risk of ICH manifold [2,3].
MRI techniques such as T2-weighted gradient echo is frequently used to diagnose acute and chronic intra-cerebral bleeds, including micro bleeds [4]. Digital Subtraction Angiography (DSA) is an essential radiological tool to rule out arterio-venous malformations, aneurysms [5]. Although, intra cerebral bleeds have been reported in patients with HIV in the past, it is rare to have multiple bleeds (acute/sub acute/chronic) in the same cerebral hemisphere. This probably suggests that the new onset hypertension in addition to the existing underlying HIV Vasculopathy, could have been the most likely etiology behind these multiple, unilobar bleeds [6,7].
a) Intracerebral Hemorrhages (ICH) is less frequent cause of stroke than cerebral ischemia in patients with retroviral disease.
b) HIV associated Cerebral Amyloid Angiopathy should be considered as the possible cause for ICH after ruling out other causes such as AVM, Aneurysmal rupture, Primary CNS Lymphoma.
c) T2 -weighted gradient-echo MRI is a useful for diagnosing older hemorrhages/micro bleeds
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
Juniper Publishers: A Leading Open Access Platform for Global Research in 2025 Juniper Publishers: A Leading Open Access Platform fo...