Juniper Publishers- Open Access Journal of Case Studies
Pigmented Condylomata Acuminata Seborrheic Keratoses -Like
Authored by Elharrouni Alaoui A
Letter to the Editor
It is difficult to distinguish condyloma acuminatum from seborrheic keratoses (KS) and bowenoid papulosis when condyloma acuminatum exhibits pigmented lesions [1,2]. We here in report a case of a seborrheric keratosis -like pigmented tumor lesion of condyloma acuminatum in the pubic
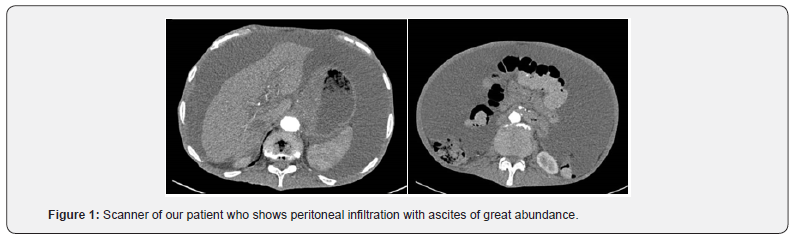
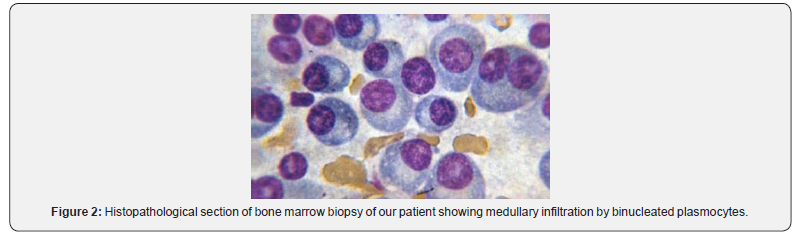
A 32-years-old man, with no significant past medical history and a normal prior sex activity. He presented with a 4-year history of pigmented asymptomatic lesions in the genital area. The clinical examination revealed pigmented tumor and well demarcated plaque at the base of the sup pubic area, measuring 2 × 3cm with papillomatous surface. The dermoscopic examination showed crypts and brain-like appearance (Figure 1). There was no evidence of lymph node enlargement and the rest of the clinical examination was normal. The patient was deeply frustrated because of the absence of sexual intercourse with his wife since the manifestation of the lesions. The diagnosis of condyloma acuminata, basal cell carcinoma, melanoma and SK were evoked.An examination of human immunodeficiency virus, syphilis, hepatitis B, and hepatitis C proved negative. The patient was taken to shaving excision of the lesion under local anesthesia. The histopathological examination of the lesions showed revealed papillomatosis and acanthosis, a high-power view demonstrated a slightly the koilocyte with disordered arrangement of keratinocytes without atypia. Based on the clinical, dermoscopic and histopathological findings, a diagnosis of pigmented condyloma acuminata KS like was made. No recurrence was observed during a 3 - month follow-up.
Condyloma acuminata (CA) is a benign tumor primarily caused by infection with HPV type-6 or type-11. CA may present with a variable clinical picture. Typical cases of CA can be easily diagnosed based on the clinical features alone [2]. Polypoid or verrucous lesions in the genitofemoral area may be harmless seborrheic keratoses or contagious condyloma acuminata [1]. A solitary lesion is particularly difficult to diagnose clinically, requiring pathological evaluation. The existence of pigmented papules of condylomata acuminata has been rarely described [3]. Herein we present a case of Pigmented condylomata acuminata with unusual clinical features in the inguinal area mimicking Giant Seborrheic Keratosis. In our case, the nodules on the mons pubis were similar to the pigmented papular lesions in CA. However, the pigmented tumor-type lesions seen in our patient have so far only rarely been mentioned in the published work [3].
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php