Juniper
Publishers-Open Access Journal of Case Studies
Scrambler Therapy and Transcranial Magnetic Stimulation: A Case Report of Varying Pain Reduction in Two Patients
Authored by Ricardo A Cruciani
Abstract
Peripheral nerve stimulation via scrambler therapy is a neurostimulative technique that may improve chronic neuropathic pain. Repetitive transcranial magnetic stimulation (rTMS) works by a different mechanism than scrambler therapy; however, this therapy is also successful in alleviating chronic neuropathic pain. Two patients with complex regional pain syndrome (CRPS) were treated for pain via scrambler therapy. When scrambler therapy was found to be ineffective, these patients were treated with repetitive transcranial magnetic stimulation. Each of these patients experienced pain relief when treated with rTMS. Comparing the course of treatment for two patients with CRPS may further guide clinicians in determining the appropriate neurostimulative therapies for given situations.
Keywords: Scrambler therapy; Repetitive transcranial magnetic stimulation; Complex regional
Introduction
Complex regional pain syndrome (CRPS) is characterized by autonomic and inflammatory changes, leading to spontaneous chronic pain [1]. One promising treatment for neuropathies, like CRPS, is scrambler therapy. This non-invasive cutaneous electrosimulation technique works to reduce pain by overwhelming the nerve fibers in the area of pain with “non-pain” signals [2]. Among alternative stimulation therapies for chronic pain is repetitive transcranial magnetic stimulation (rTMS); rTMS involves placing a coil that produces magnetic fields over targeted areas of the brain [3]. These magnetic fields are then able to induce depolarization or hyperpolarization of neurons which in turn causes the firing of action potentials. The mechanistic differences between peripheral nerve stimulation and the electromagnetic induction of rTMS likely play a role in the varying clinical efficacies observed for the treatment of pain [4].
This case report highlights two patients for which scrambler therapy failed to diminish pain ratings, however, treatment with rTMS succeeded. This analysis identifies individual factors that may have contributed to the observed differences in treatment efficacy. Some of these factors include gender, age, diagnosis, location of pain, years of pain, medications taken during the course of treatment and number of treatment visits. Calling attention to the differences and similarities in each of these cases may help guide future research that compares stimulative therapies used to treat neuropathic pain [5].
Case Presentation
Case 1
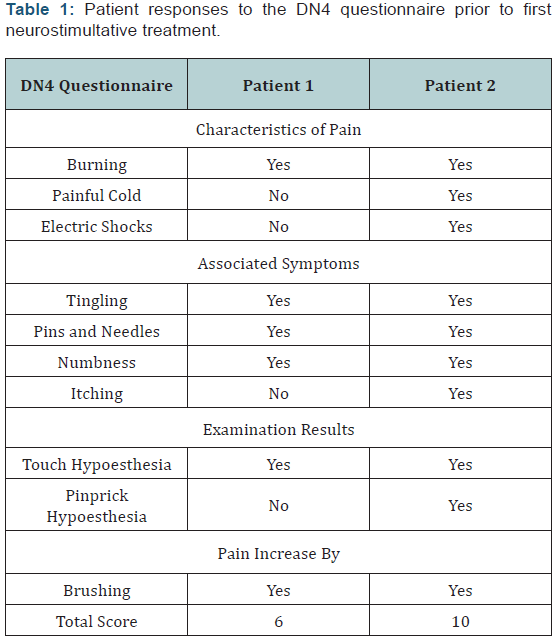
Patient 1 is a female, who was 36 years old at the time neurostimulative therapy began. She was diagnosed with Type II CRPS in her right upper extremity that began 2 years prior to treatment in 2014. In early 2012, the patient was diagnosed with a herniated disk of the cervical spine, eventually prompting a C5 diskectomy. However, following “failure of hardware,” elective surgery for the removal of a screw at C6 was performed. Post-operatively, this patient developed right upper extremity palsy likely related to a right vertebral artery occlusion. Despite resolution of the right upper extremity palsy, severe pain remained in this location. Her pain can be characterized primarily by “burning,” “numbness,” and “pins and needles” (Table 1).
Following a course of unsuccessful pharmacological interventions, this patient was identified as a candidate for scrambler therapy. She completed 11 treatment visits, occurring in the following pattern: 5 consecutive days, two off days, 5 consecutive days, 3 off days and one day. During these treatments, electrodes were placed on her right upper arm, forearm, hand, neck and shoulders. No significant change in blood pressure or heart rate was observed over the course of each treatment session. A rating was obtained from the patient prior, 15-20 minutes into and post-stimulation. A diary with pain intensity ratings was kept rigorously over the course of the treatment. The Numerical Pain Rating Score (NRS) was used to gather pain intensity.
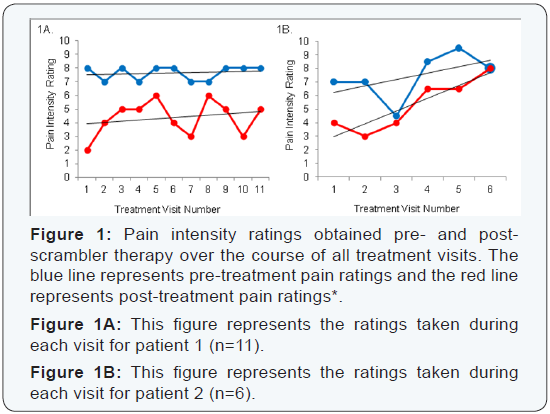
Concomitant medication included diphenhydramine, pregabalin, duloxetine HCl, hydromorphone HCl, zestril, lubiprostone. Negative, yet tolerable, side effects were experienced during several treatment visits. These side effects included neck strain, full body sweating, exhaustion, burning in quadriceps and migraines. Ultimately, scrambler therapy did not provide a great amount of pain relief as indicated by the NRS pain ratings taken pre- and post-stimulation (Figure 1A). Further, the difference in pre- and post-pain ratings decreased over the course of treatment. Due to the unsuccessful course of scrambler therapy, the patient opted to undergo rTMS for her chronic neuropathic pain. She completed 36 treatment visits, occurring over the course of approximately 3 months. During these treatments, her right arm was targeted through stimulation of the corresponding motor strip in the brain. No significant change in blood pressure or heart rate was observed over the course of each treatment session. Again, a rating was obtained from the patient prior, 15-20 minutes into and post-stimulation.
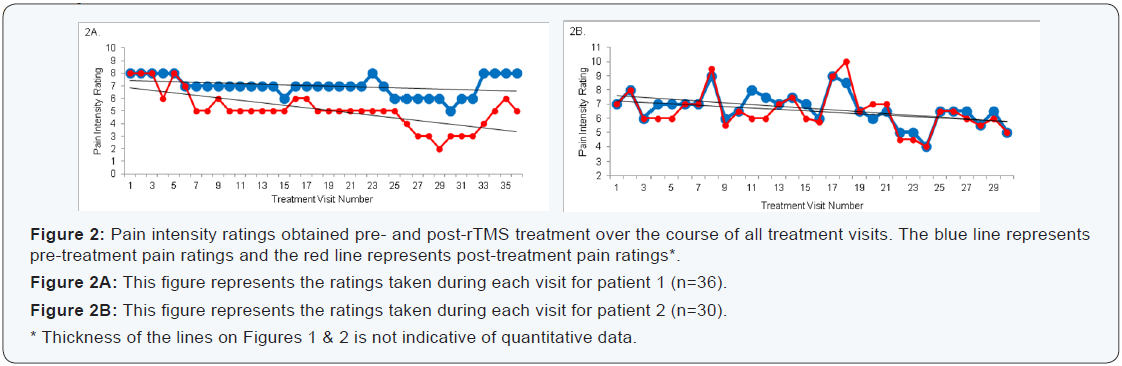
A diary with pain intensity ratings was kept rigorously over the course of the treatment. The Numerical Pain Rating Score (NRS) was used to gather pain intensity. Concomitant medication included rizatriptan benzoate, ultram, ropinirole HCl, sertraline HCl, zestril and desyrel. At treatment visit number 13 the patient was additionally prescribed ketamine HCl and hydromorphone HCl. At visit number 23, tizanidine was added to her medication regimen. No side effects were experienced during treatment visits. Ultimately, rTMS did provide pain relief as indicated by the NRS pain ratings taken pre and post-stimulation (Figure 2A). Further, the difference in pre- and post-pain ratings increased over the
Case 2
Patient 2 is a female who was 28 years old at the time neurostimulative therapy began. She was diagnosed with Type I CRPS in her right upper extremity that began 2 years prior to treatment in 2015. The onset of pain was sudden. The patient suggests her general cause of pain is work-related. Her work involved repetitive movement and lifting. Pain relief therapies including acupuncture, chiropractic care, physical therapy and multiple medications were attempted. A cervical spine MRI performed late in 2014 shows this patient to have multilevel spondylosis; however, no acute abnormality. Early in 2015, the patient underwent cervical epidural steroid injection to treat her unchanged midline and bilateral neck pain radiating to the right shoulder in addition to right wrist pain, numbness and tingling in right hand. A follow-up several months later revealed no change in pain.
The patient characterized many symptoms related to pain that included weakness in affected areas that interfered with sleep, changes in coloration and sensitivity to soft touch. At this time, the allodynia was identified at its most intense in the right shoulder and neck area (Table 1). Following many unsuccessful interventions, this patient was identified as a candidate for scrambler therapy. She completed 6 treatment visits, occurring in the following pattern: 5 consecutive days, two off days and one day. During these treatments, electrodes were placed on her right neck and shoulder. No significant change in blood pressure or heart rate was observed over the course of each treatment session. A rating was obtained from the patient prior-, 15-20 minutes into and post-stimulation. A diary with pain intensity ratings was kept rigorously over the course of the treatment. The Numerical Pain Rating Score (NRS) was used to gather pain intensity.
Concomitant medication included pamelor, pregabalin, oxycodone acetaminophen and hydromorphone HCl. No side effects were experienced during several treatment visits. Ultimately, scrambler therapy did not provide pain relief. In fact, the NRS pain ratings taken pre- and post-stimulation indicated a slight increase in pain (Figure 1B). Further, the difference in preand post-pain ratings decreased over the course of treatment.
Due to the unsuccessful course of scrambler therapy, the patient opted to undergo rTMS for her chronic neuropathic pain. She completed 30 treatment visits, occurring over the course of approximately 1 month. During these treatments, her right arm, hand, shoulder and neck were targeted through stimulation of the corresponding motor strip in the brain. No significant change in blood pressure or heart rate was observed over the course of each treatment session. A rating was obtained from the patient prior-, 15-20 minutes into and post-stimulation. A diary with pain intensity ratings was kept rigorously over the course of the treatment. The Numerical Pain Rating Score (NRS) was used to gather pain intensity. Concomitant medication included pamelor, pregabalin, oxycodone acetaminophen and hydromorphone HCl. No side effects were experienced during treatment visits.
Ultimately, rTMS did provide some momentary pain relief as indicated by the NRS pain ratings taken pre and post-stimulation (Figure 2B). Further, the difference in pre and post-pain ratings slightly decreased over the course of treatment.
Discussion
In the cases considered both patients were middle aged females diagnosed with CRPS localized to the right upper extremity. The current body of research suggests that CRPS can be considered a neuropathic pain condition and divided in to two sub-groups, type I and type II. Type II CRPS can be distinguished by an evident peripheral nerve injury, while the cause of type I is typically more difficult to identify [6]. Evidence suggests that both forms of CRPS work by a multifaceted mechanism involving both the central and peripheral nervous system [7]. While each of these patients was diagnosed with a different type of CRPS, their treatment courses were similar. Because both women failed to respond to traditional pharmacological treatments and surgical interventions, neurostimulation was prescribed. Varying responses to stimulation in these two cases may help further the understanding of CRPS’s mechanism, ultimately aiding clinicians in effectively developing mechanism based treatments for the condition.
The first neurostimulative technique prescribed in these cases, scrambler therapy, works through cutaneous and direct stimulation of the area in pain. This therapy has been shown to significantly decrease neuropathic pain; one study found an average pre-treatment rating of 7.41 on the Numerical Pain Rating Scale (NRS) dropping to 1.60 post-treatment [8]. Despite early success in treating pain, the mechanism of scrambler therapy is not fully understood, prompting further research. Thus, when scrambler therapy resulted in a lack of pain reduction and/or mild side effects, a different type of stimulation was considered. Several alternative stimulation therapies exist for treating chronic neuropathic pain; among these treatments is repetitive transcranial magnetic stimulation (rTMS) [3]. For each of the presented cases, subsequent rTMS treatment courses were similar in number of stimulation visits. The patients in case 1 and 2 attended 36 and 30 visits, respectively. However, the length of time between visits varied greatly for each of these patients. The rTMS treatment course used in case 1 occurred over 3 months, whereas the course in case 2 occurred of 1 month. More pain relief over a longer period of time was achieved in case 1, suggesting that length of treatment course may affect efficacy and longevity of pain relief achieved by rTMS.
This case study shows that, for a given circumstance, certain neurostimulative therapies may be more successful than others [9]. For two young female patients presenting with two years of CRPS in their right upper extremity, rTMS over a period as long as 3 months better resolved pain symptoms than scrambler therapy. Future critical analysis of demographic factors, pain type, pain location, years of pain and length of treatment may provide preliminary insight into the mechanistic differences between the therapies that result in varying responses, allowing physicians to choose appropriate therapies for chronic neuropathic pain relief.



No comments:
Post a Comment