Juniper Publishers-Open Access Journal of Case Studies
Postmenopausal Osteoporosis
Authored by Vikram Khanna
Abstract
Osteoporosis is a condition with a very high prevalence and its spreading at a rapid pace which is in tandem with the increase in the life expectancy of the general population. With the change in the eating habits the patients are not getting adequate nutrition for the wellbeing of the bones. With the advancements in the field of bone mineral density measurement it may now be possible for early detection and rapid treatment which may lead to the better outcome for the patient and may prove less detrimental for the society as well.
Keywords: Osteoporosis; Menopause; BMD
Introduction
Osteoporosis is a silent condition which has been on the rise in the recent times due to the increase in the life expectancy of the patients [1]. This affects the physical, mental as well as socioeconomic condition of the patient. This review article summarizes the important aspects of this condition as well as sheds light on its treatment.
Definition
The working group of WHO in 1994 came up with the definition which was based on T score of the Bone mineral density (BMD) and it said that a T score less than -2.5 can be considered as osteoporosis [2].
Background
The number of patients with osteoporosis is on a rise and it is expected that the no. will soon reach 34 million in USA [3]. Out of which 80% are expected to be women. The incidence of osteoporosis increases exponentially with age and there is a sharp increase in cases following menopause in females. The incidence of osteoporosis is also associated with an increase in the incidence of fractures which also rises following the decrease in the bone mineral density [4].
Pathophysiology of Postmenopausal Osteoporosis
There may be 2 causes of postmenopausal osteoporosis
- Low peak bone mass
- Increased bone loss, or both Peak bone mass is determined 70%-80% by genetic factors [5-8]. Remaining causative factors for the peak bone mass include factors like nutrition, activity and hormonal interplay.
Once the peak bone mass is achieved, bone regulation takes place by local remodeling which is regulated by RANK, RANKL protein and OPG. RANK or receptor activator of nuclear factor-kb is present in the osteoclasts and causes the increase in their activity. RANKL or the RANK Ligand is synthetized by osteoblasts and it binds with the RANK receptor on the osteoclasts. OPG or Osteoprotegerin is also synthetized by the osteoblasts and prevents the binding of the RANK to the RANK Ligand by itself binding to the RANKL. Hence, the activity of the osteoclasts and in turn the bone remodeling depends upon the interplay between the RANK and the OPG. This interplay is controlled by hormonal and local factors. If the bone remodeling is in balance (osteoblast = osteoclasts) then there is no decrease in the BMD. A change in the balance of remodeling causes the change in the BMD accordingly.
In postmenopausal females, there are hormonal changes which cause an increase in the RANKL which causes increase in the osteoclastic activity and hence, shifts the bone remodeling towards a bone resorbing balance which leads to osteoporosis.
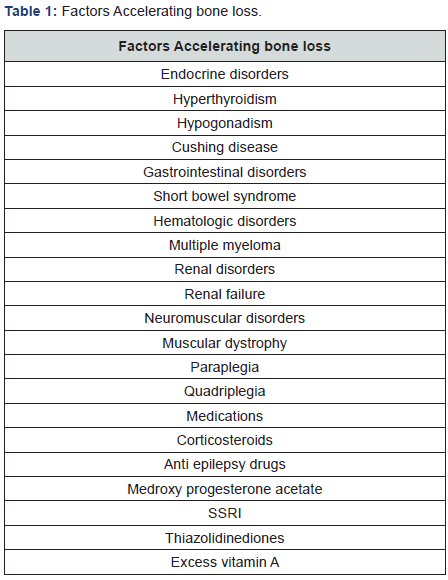
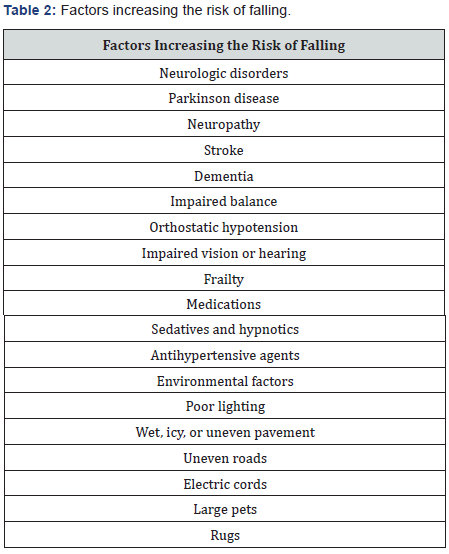
It has been noted that the bone loss is maximum 3-5 years before menopause and also 3-5 years after menopause. These points towards the indirect as well as the direct causes of bone loss leading to osteoporosis. This bone loss is faster than the average bone loss seen in the senile osteoporosis seen in males. There is also research going on which suggests the change in the micro architecture of bone with the advent of osteoporosis. However, this research and the quantification of these changes are still in experimental stages and not available for commercial use [9]. Factors which accelerate bone loss are included in Table 1. Also, factors which increase the risk of falling and fractures are included in Table 2.
Clinical Features of Postmenopausal Osteoporosis
These include:
- Low Bone mass: measured by BMD
- Fracture: Single most important manifestation of postmenopausal osteoporosis.
Lifestyle and Non pharmacologic Measures for Bone Health
Goals of this therapy include:
- Optimizing skeletal development to increase the peak bone mass
- Prevent secondary bone loss
- Preserve the skeletal structural integrity
- Prevent fractures
Following diets should be taken into consideration:
- Good general Nutrition: A balanced diet is necessary for the development of a good peak bone mass. The peak bone mass also depends upon the protein intake as well as the activity level of the patient [10-12].
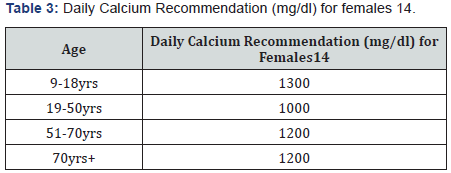
- Calcium: The recommended dose of daily requirement of calcium in various situations is given in Table 3. Some points to be taken into consideration are that calcium is absorbed better with food and calcium citrate gives the least amount of GI side effects as compared to other calcium compounds.
- Vitamin D: It is important to assess serum Vitamin D in all individuals suffering from osteoporosis. Vitamin D is found in food stuff like fish oils, fortified milk, cereals and breads. National Osteoporosis foundation recommends a dose of 800-1000 IU for patients more than 50 years old [13]. However, many experts feel that the dose should be between 1000-2000 IU (Safe upper limit being 4000IU/day) [14]. Currently the normal level is 30-32ng/ml (Upper limit being 60ng/ml) [15]. Even though daily doses are present still it has been seen that the intermittent dose was found to be 3 times more potent [16].
- Other dietary supplements: Magnesium doesn’t increase the calcium absorption but decrease the GI side effects [17]. Excessive Vitamin A was harmful for the bones in large doses (more than 100000 IU) [18]. Vitamin K (1mg/ day) has been found to decrease the bone turnover and hence decrease the bone loss [19]. Natural estrogens (isoflavones) were thought to prevent bone loss but there has not been any scientific evidence for the same [20-22].
- Alcohol: Excessive alcohol intake causes bone loss [23]. Postmenopausal women should take a maximum of 7 drinks a week.
- Caffeine: Postmenopausal osteoporotic women should limit their caffeine intake less than 1-2 servings/day as it decreases the intestinal absorption of calcium [24].
- Smoking: It is associated with osteoporotic fractures. Patients who give up smoking are at a lesser risk than those who are active smokers [25].
- Exercise: Regular light exercises (30-40 mins) everyday increases the muscle strength and it has been seen that it also causes the bone strength to increase [26,27]. However patients with severe osteoporosis should avoid heavy exercises like lifting weights or excessive pushing or pulling.
Prevention of risk factors for Post-menopausal osteoporosis
- Spine Imaging: to rule out any fractures
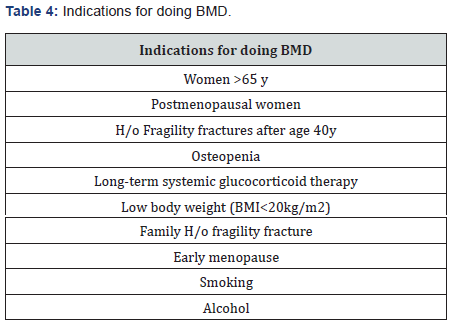
- BMD: measured either at the spine or the neck of femur. It can be used to assess the probability of fracture in the next 10 years in a patient using the FRAX tool. However, this modality is still expensive and the benefit to the society is still not confirmed. Lists of indications have been summarized in Table 4.
Treatment of Osteoporosis
Candidates requiring treatment for osteoporosis include [28]:
- Hip or spine fracture
- T score <-2.5
- T score between -1 to -2.5 with a probability of fracture as calculated by FRAX tool
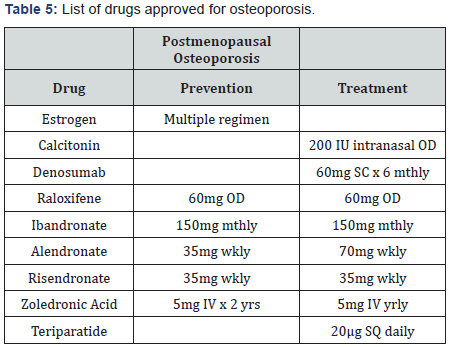
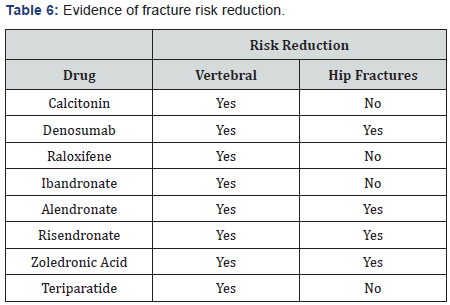
Drugs approved for postmenopausal osteoporosis have been listed along with their dosage in Table 5 and their possible effects on fracture risk reduction have been mentioned in Table 6. Concomitant use of anti-osteoporotic drugs was thought to reduce the fracture risk better than using a single drug [29]. However, further studies have led to the non-recommendation of this practice [30]. The sequential use of drugs, first the anabolic group followed by the anti resorptive drugs has been found to be beneficial for patients [31].
BMD in progression of the treatment
BMD may be used for the prognosis and the follow-up of the treatment of osteoporosis. The treatment is said to have failed if there is substantial fall in the BMD or any fracture occurrence.
Operative treatment for osteoporosis
Most commonly occurring fractures are the vertebral fractures and there has always been a difference of opinion regarding the management of the same. Vertebroplasty though decreases the pain instantly but doesn’t increase the vertebral height to normal whereas, Kyphoplasty increases the vertebral height along with the reduction in the pain but is expensive [32- 36]. The surgeon should be careful in the fixation of the other fractures by using locking plates and HA coated implants to provide a stable fixation.
Conclusion
The incidence of postmenopausal osteoporosis is on the rise and one should be careful in the management and suitable pharmacotherapy should be given which is tailor made for each and every patient.
For more Open Access Journals in Juniper Publishers please click
on: https://juniperpublishers.business.site/
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jojcs/JOJCS.MS.ID.555570.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jojcs/JOJCS.MS.ID.555570.php



No comments:
Post a Comment