Juniper Publishers- Open Access Journal of Case Studies
Crohn’s Disease-Walking Towards a Cure
Authored by Mohamud A Verjee
Abstract
Crohn’s disease (CD) has a well-established reputation as an autoimmune, inflammatory bowel disorder, usually requiring pharmacological therapy for control. Affecting mainly the terminal ileum, CD can affect any part of the gastrointestinal tract. It usually appears in patches and can extend through the entire thickness of the colon wall. Remission with medication is achievable, but over two-thirds of patients relapse within five years. Intractable, active CD affects the quality of life of an individual and pervades every aspect of health, often with multi-organ involvement. Included are joints, skin, eyes, and blood. While the cause of CD is multifactorial, hemopoietic stem cell transplantation (HSCT) provides a possible answer for control of the disease. Modified non-myeloablation regimes show great promise with improved survival rates, reduced symptoms, or full remission.
Keywords: Crohn’s disease; Hemopoietic stem cell transplantation; Myeloablation; Non-myeloablation; Remission; Bone marrow
Abbreviations: ACCA: Anti Chitobioside; ALCA: Anti-Laminaribioside; AMCA: Anti-Mannobioside; Anti-L: Anti-Laminarin; Anti-C: Anti-Chitin; Anti-OmpC: Anti-Outer Membrane Porin C; Anti-TNF: Anti-Tumor Necrosis Factor; ASCA: Anti-Glycan Antibodies; Anti Saccharomices Cerevisiae; CBC: Complete Blood Count; CD: Crohn’s Disease; CDAI: Crohn’s Disease Activity Index; CT: Computerized Tomography; CRP-C: Reactive Protein; ESR: Erythrocyte Sedimentation Rate; FOB: Fecal Occult Blood; GAB: Goblet Cell Antibodies; GI: Gastrointestinal System; HSCT: Hemopoeitic Stem Cell Transplantation; MRI: Magnetic Resonance Imaging; PAB: Autoantibodies Targeting the Exocrine Pancreas; PET-CT: Positron Emission Tomography + Computerized Tomography; PET-MR: Positron Emission Tomography + Magnetic Resonance Imaging; pANCA: Anti-Neutrophil Cytoplasmic Autoantibodies; SBE: Small Bowel Enteroclycis; SBFT: Small Bowel Follow Through; TIBC: Total Iron Binding Capacity; WBC: White Blood Cells
Introduction
A 28-year-old male attended the Emergency Department of a tertiary care hospital with an acute onset of left sided lower abdominal pain. The patient’s previous history confirmed several previous acute episodes of CD, all treated aggressively. The patient’s disappointment with all the treatment to date resulted in a refusal to accept more medication. He expressed his view vociferously. “I do not want any more medicines. I can’t stand any more hospitalizations. I need a cure!”
CD or regional ileitis is an idiopathic, immune-mediated, chronic inflammatory bowel disorder that can involve the entire gastrointestinal tract from mouth to anus. Most cases of CD affect the small intestine, particularly the terminal ileum, three times more than the jejunum and the rest of the small bowel [1].
Epidemiology
The highest incidence of CD occurs in the United Kingdom in Caucasian women after one year’s use of the contraceptive pill, at twelve cases per 100,000. In the United States, the average rate of incidence of CD varies from seven cases per 100,000 to twenty in smokers [2]. The peak ages of onset are bimodal at 15-30 years and 60-80 years [3]. The prevalence is highest amongst populations of Jewish ancestry.
Etiology
Genetic, environmental, microbial, immunologic, and dietary factors are involved in the development of CD. Monozygotic twins studied with the disorder show 58% concordance. Linkage analysis and genome wide association studies reveal a hundred disease-associated loci on different chromosomes. Smoking, oral contraceptives, and non-steroidal anti-inflammatory drugs all feature in precipitating the illness.
Pathogenesis
In genetically predisposed individuals, several endogenous and exogenous factors interact to produce a dysfunctional mucosal inflammatory reaction, further modified by environmental factors.
The dysregulated response of the T-helper lymphocyte predominates in CD. Cytokine-activated inflammatory cells release several inflammatory mediators precipitating injury to the intestinal mucosa. The initial intestinal inflammation is commonly from superficial ulcerations that progress into deeper layers, involving the entire colonic mucosa and affecting regional lymph nodes, in the form of non-caseating granulomas.
Clinical Presentation
Numerous signs and symptoms typify the disorder. Not all need to be present but pain, weight loss, fatigue and diarrhea are common denominators. The patient experienced all of the above signs and symptoms.
Intestinal manifestations to elicit
- Abdominal pain.
- Weight loss.
- Fatigue.
- Intermittent diarrhea.
- Low-grade fever.
- Post prandial pain.
- Hematochezia.
- Anal fissure.
- Anorexia, nausea, and vomiting.
Extra-Intestinal manifestations include
- Arthritis and arthralgia.
- Sweet syndrome.
- Angular and aphthous stomatitis.
- Acrodermatitis enteropathica.
- Episcleritis and anterior uveitis.
- Pyoderma gangrenosum.
- Nephrolithiasis.
Work-Up and Diagnosis
- Laboratory investigations include
- Complete blood cell count (CBC).
- Chemistry panel(lytes, albumin, Fe, TIBC, Ca2+, Mg2+, Vit B12, folate, liver function (monitoring sclerosing cholangitis).
- Inflammatory markers (CRP, ESR).
- Stool analysis (WBC, FOB, pathogens, ova, parasites, C. difficile).
- Serologic markers (antibodies: ASCA, ALCA, ACCA, AMCA, anti-L, anti-C, anti-OmpC, PAB, pANCA.
These markers cover all those that might be associated with CD and ulcerative colitis (UC), including situations where the disorder is not clearly delineated.
According to Casciani et al. [1] more than 20% of all CD patients present before 18 years of age. Imaging studies are various, with every attempt to reduce exposure to ionizing radiation, especially in children and adolescents. They include
- Plain x-ray.
- Barium studies-small bowel enteroclysis (SBE) or follow-through (SBFT).
- Ultrasonography.
- CT scan.
- Upper GI endoscopy.
- Ileocolonoscopy and ultrasound.
- Magnetic resonance imaging (MRI).
- PET-CT.
- PET-MR (Predicted for the future [1]).
Management
Medical therapy includes
- Immunomodulators and monoclonal antibodies (e.g. Azathioprine, Methotrexate, mercaptopurine).
- Biologic anti-TNF therapy (Infliximab, adalimumab, certolizumab).
- Corticosteroids (high dose).
- Immunosuppressive therapy (Cyclophosphamide; antithymocyte globulin).
- Antibiotics (Ciprofloaxacin, Metronidazole).
- Anti-diarrheal medication (Loperamide, Diphenoxylate, codeine sulfate).
- Nutritional supplements (Iron, Vit B12, folic acid).
- Bile acid sequestrates (Cholestyramine).
Surgical therapy
Indications for invasive surgical intervention include
- Persistent symptoms despite medical treatment
- Fistulae formation and other complications.
- Bowel resection for malignancy (lymphoma).
- Consideration of small bowel transplantation.
Is There a Cure?
Hematopoietic stem cell transplantation (HCST): Multipotent, healthy, hemopoietic stem cells arise from bone marrow, peripheral, or umbilical cord blood. They can be autologous or allogeneic. Stem cells can be syngeneic between identical twins. When certain cancers such as leukemia or multiple myeloma are involved, patients are subjected to immunosuppression through intense chemotherapy or radiation treatment before receiving a stem cell transplant. The main problems arising are graft vs. host reactions, and significant infection due to immunosuppression. The procedure extends to autoimmune diseases [1] among other rare disorders.
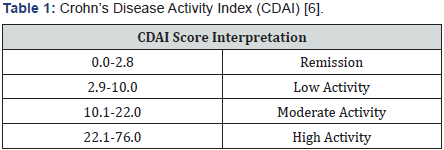
Hematopoietic stem cell transplants [4,5] are saved for patients with the severest expression of disease, who fail standard therapy, most likely with anti-tumor necrosis factor refractory disease, and whose Crohn’s Disease Activity Index (CDAI) exceeds 250 [6]. The duration of remission after treatment is still uncertain. A fall in the CDAI to below 150 signifies remission. The Harvey-Bradshaw index [7] arose for data collection in 1980, and a simpler clinical assessment CDAI followed later in 1980 [8].
(Table 1) [6].
The first successful hematopoietic stem cell transplantation was at Northwestern University in Chicago, in 2001[3]. Twenty-two patients underwent hematopoietic stem cell transplantation, with 80% achieving total remission, and 20% markedly improved in their quality of life.
Burt et al. [9,10] in 2010 evaded irreversible bone marrow failure by using modified non-myeloablative protocols, which halted destructive inflammation, enabling the bone marrow to recover. Immunosuppressive drugs are needed for the rest of life, as bone marrow is rendered inactive by myeloablation. Following a non-myeloablative regimen, autologous stem cells are infused as a supportive blood product to hasten recovery and shorten duration of neutropenia and cytopenia [9,10].
Lindsay et al. [11] completed unmasked treatment with randomly assigned patients, but masked adjudicators in assessing outcomes (ASTIC Trial). Treatment related infection was the main complication, as well as worse outcomes in smokers. They suggested therapy “be targeted to patients most likely to benefit.”
Conclusion
The patient was lost to follow up. Seeking another treatment center or carer were possible reasons. HSCT techniques have improved clinical outcomes in CD and show endoscopic benefit but may cause significant side effects. Careful selection of patients with appropriate counseling seems more prudent rather than regarding HSCT as another option for treatment, although some patients may enquire about, or insist on other forms of treatment, when they have tried everything else on offer.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment