Juniper Publishers- Open Access Journal of Case Studies
Seal it to Heal it-Management of Side Branch Perforation with Autologous Clotted Blood
Authored by S Mehrotra
Abstract
Coronary perforations (CP) are rare but feared complications of coronary interventions [1-4]. Treatment of guidewire-induced CP (GW-CP) is challenging because they may be associated with catastrophic clinical consequences if unsuspected or poorly managed. We report a patient whose intervention was complicated by coronary perforation due to balloon inflation in a small branch of the left cirumflex coronary artery (LCX). Blood extravastion to the pericardium was stopped by embolisation of the artery with patients own blood, thereby avoiding the need for emergent cardiac surgery.
Keywords: Coronary perforation; Dual catheter technique; Autologous clotted blood
Presentation of the Case
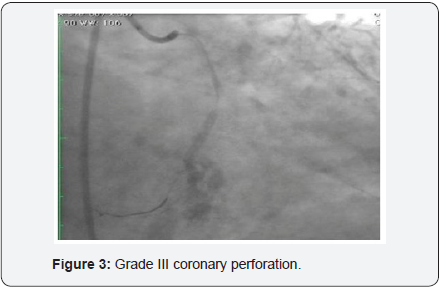
60-year-old hypertensive male had presented with recent onset NYHA class II angina. The electrocardiogram (ECG) showed ST depression and T wave inversion in leads V1-V4. The 2-D echocardiogram revealed normal LVEF (60%) with no wall motion abnormality. Coronary angiography revealed a tight 90% stenosis in Mid LAD (Left anterior descending) and a total occlusion of proximal LCX (Figure 1). The patient underwent PCI after an informed consent. The patient was given 600mg clopidogrel one day prior and 5,000U intravenous heparin was given at the start of the procedure. According to the clinical setting and electrocardiogram changes, LAD was considered to be the culprit vessel with CTO (chronic total occlusion) of LCX. The left main was engaged with 6 Fr EBU 3 (Cordis Co., USA) and PCI (percutaneous coronary intervention) of LAD was performed with a DES (drug eluting stent) with good angiographic result. The LCX occlusion was crossed with Sion Blue wire (Asahi Intecc Co., Japan). The wire however slipped into one of the small side branches which was mistaken to be the main vessel. Predilatation with wire in a small branch with a 2.5 X12mm, Emerge, (Boston Scientific, Natick, MA) (Figure 2) resulted in a grade III C.P (Figure 3). Mechanical hemostasis was accomplished by inflating the same predilatation balloon in the main branch proximal to the perforation. Multiple inflations were performed at low atmospheres for 4-5min. However extravasation of contrast medium to the pericardium persisted necessitating reversal of heparin by administering 5mg of Protamine. The leaking LCX branch had to be now targeted for occlusive treatment and for which intra-coronary injection of autologous clotted blood was considered, as other embolic materials like gel foam, collagen and coils were not available on the shelf.
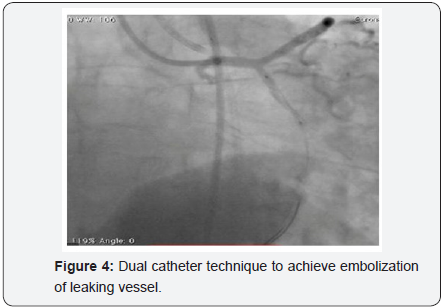
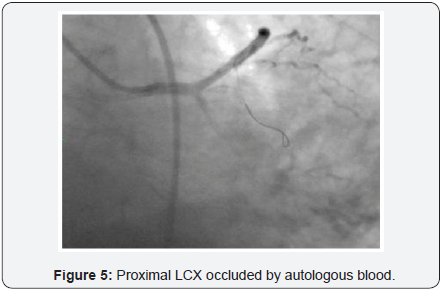
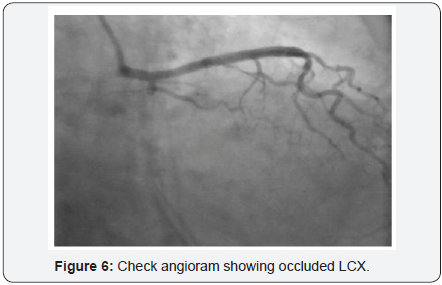
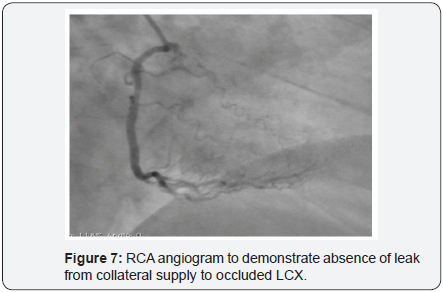
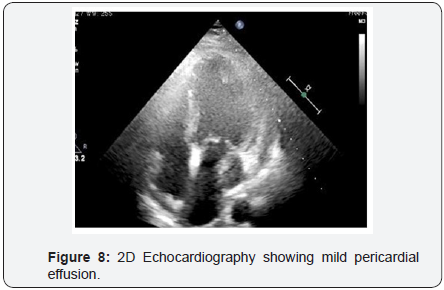
To decrease extravasation time during autologous blood embolisation, the left common femoral artery was accessed with a 6Fr sheath and a 6Fr EBU 3 guide catheter was advanced and placed adjacent to the 6Fr guide catheter at the LM ostium (Figure 4). This sequence of events was performed in approximately 4min and prevented the development of tamponade. A sion blue wire was then passed into the distal LCX with transient balloon deflation to allow wire passage. Autologous clotted blood injected through the aspiration thrombectomy (Pronto LP, Vascular Solutions, Minneapolis, MN) catheter was used to embolise the leaking vessel. The balloon was kept inflated during injection of clotted blood to prevent back leak. The LCX artery occluded instantaneously at proximal level with immediate stoppage of the leak into the pericardium .There was an excellent final result (Figure 5) and the absence of extravasation was confirmed in a repeat angiography (Figure 6). RCA (right coronary artery) angiogram was also taken (Figure 7) which did not reveal any leak from the collateral supply to the occluded LCX. The ECG showed Q waves in I, AVL and troponin values were positive. The following morning, the echocardiogram showed mild pericardial and pleural effusion (Figure 8) and the patient was discharged at 72hrs with a subsequent uneventful course.
Discussion
The frequency of coronary perforation ranges from 0.19% to 3.0% [2,5-8], 0.1% in balloon angioplasty and 0.5-3% in procedures involving the so called newer devices. Risk factors for perforation include complex coronary anatomy (Type B2 and C lesions), chronic total occlusion, rotational atherectomy and intravascular ultrasound use [3]. The in-hospital outcome after perforations is complicated by death in about 10%, myocardial infarction in 19%-34% and emergency surgery in 12%-39% [9]. Vessel occlusion, intramyocardial hemorrhage, and the development of cardiac tamponade, mainly determine the clinical outcome in patients with coronary perforation
Therapeutic measures for management depends on the type of perforation as well as its location. A perforation in the proximal part of a vessel can be managed with prolonged balloon inflation [1,10] or with the deployment of covered stent, provided there is no side branch at the site of perforation. However in a location at a distal segment or branch of a vessel as in the index case, in addition to prolonged balloon inflation, embolization of the leaking vessel is the therapeutic goal to stop the leak at the cost of inducing an iatrogenic infarction. There are several reports describing the usefulness of subcutaneous fat, coils, gel foam and thrombin for the treatment of side branch perforation [11- 14]. However, there are few reports describing the treatment of side branch perforation as in the present case with autologous clotted [15-17] blood.
Autologous blood clot is made by stirring blood gathered from the sheath and when left to stand, the clot is easily divided into a hard thrombus and fragile thrombus. The time required for the blood to become of thick consistency was approximately 15 minutes, and was probably related to the anticoagulation level at that time. The advantage of autologous clotted blood over other agents is that it is safe, cost effective and can be obtained easily. Most importantly, unlike other agents, embolization with clotted blood is reversible and salvages the target organ [18]. The occlusion of the lumen of the vessel is unstable and easily disrupted allowing perfusion, but the clot adherent to the vessel wall remains stable, thus preventing any leak. However as the leak in our case was from a small side branch into the pericardium, disruption of intraluminal clot to maintain vessel patency was not attempted. One disadvantage is that since blood clot is formed outside the body, it may cause infection if stringent sterile precautions are not exercised during its preparation. Another concern is the risk of systemic embolization.
Conclusion
Autologous clotted blood embolization of the leaking vessel represents an alternate way to attempt nonsurgical management of coronary perforation especially in cases where the guidewire cannot be advanced beyond the site of perforation and in small vessels where prolonged balloon inflation fails and deployment of covered stent is not an option.
For more Open Access Journals in JuniperPublishers please click on:
https://www.linkedin.com/company/juniper-publishers
For more articles in Open Access Journal of Case Studies please
click on: https://juniperpublishers.com/jojcs/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jojcs/JOJCS.MS.ID.555631.php



No comments:
Post a Comment