Juniper Publishers- Open Access Journal of Case Studies
Autoimmune Hemolytic Anemia Preceding the Diagnosis of Hodgkin’s Disease: a Case Report and Review of the Literature
Authored by Didem Karaçetin
Abstract
Autoimmune hemolytic anemia (AIHA) is known to be associated with Hodgkin’s disease (HD) but is uncommon.” It has usually presented at the time of initial diagnosis of HD or during the course of the disease. Immune hemolytic anemia has been very rare in Hodgkin’s disease”. Use present perfect to emphasize your recent reported case than the previous scientific evidence. Immune hemolytic anemia is very rare in Hodgkin’s disease. In this report, we describe 68 years old male patient with Hodgkin’s disease that presented with immune hemolytic anemia.
Keywords: Autoimmune hemolytic anemia; Hodgkin ’s disease
Introduction
Hodgkin’s disease is a distinct malignant disorder of the lymphatic system and is more common in males. The age-specific incidence of the disease is bimodal, with its greatest peak in the 3rd decade of life and a second small-peak in the 7th decade. Histologic structure and the affected sites differ according to the age of the patients. Viral infection, environmental or occupational exposures and a genetically determined host response are believed to be etiologic factors of this disease. Patients usually have painless lymphadenopathy at initial presentation. Extralymphatic tissue involvement is rare. Mediastinal involvement is present in half of the patients Hodgkin’s disease (HD) classically presents with lymph node enlargement with or without ‘B’ symptoms (Unexplained weight loss exceeding 10% of body weight in 6 months, fever and drenching night sweats) [1]. Mild normocytic normochromic anemia is common at diagnosis; mild leukocytosis, monocytosis and lymphopenia may occur, but are more commonly seen in patients at advanced stages [2]. These hematological findings may occur as paraneoplastic effects of the disease or due to bone marrow involvement. Anemia is a common manifestation of Hodgkin’s disease and different mechanisms which contribute to anemia include anemia of chronic disease, reduced red cell survival, bone marrow infiltration, autoimmune hemolytic anaemia (AIHA) and bone marrow suppression by chemotherapy. The diagnosis of Hodgkin’s disease requires an expert hematopathologic interpretation of a lymph node specimen. Hodgkin’s disease has four histologic subtypes: lymphocyte predominant, nodular sclerosing, mixed cellularity and lymphocyte depletion [2]. Nodular sclerosing Hodgkin’s disease is the most common subtype and typically affects young females while the mixed-cellularity subtype is seen in the elderly. The stage of the disease is the most important determinant of treatment options, which include chemotherapy, radiotherapy or both. AIHA associated with HD is uncommon [3]. The diagnosis of AIHA is usually associated with HD at the time of initial presentation or during the course of disease [4,5]. Immune hemolytic anemia is very rare in Hodgkin’s disease, and it was first reported in 1966 [4]. In this report, we describe a case of Hodgkin’s disease that presented with immune hemolytic anemia.
Case Report
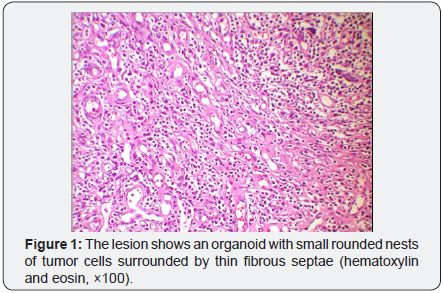
A 68 year old male, who hadn’t any comorbidite presented with a history of malaise, intermittent fever and dizziness with yellow discolouration of the sclera and dark urine of two week duration. There was no antecedent history of viral type illness or anemia. Clinical examination revealed an ill looking man with marked pallor and mild icterus and swelling of the right axiller lymph nodes. He was febrile with a temperature of 39 ºC he was pale, tachycardic, and tachypneic. Rales were heard at the bases of both lungs. Hepatosplenomegaly was present. The spleen was palpable 5cm below the left costal margin, and the liver edge was palpated 3cm below the right costal margin. Hematologic and biochemical values of the patient was: Hemoglobin 6gr/dl, MCV 99.5fl, Hematocrit 18.8%, White blood cell count 9.8x109/l, Platelet count 147x109/l, Blood urea nitrogen 63.3mg/dl, Creatinine 1.03mg/dl, LDH 868 IU/l, Direct bilirubin 4.5mg/dl, Indirect bilirubin 0.6mg/dl, ALT 27IU/l, ALT 34IU/l, Vitamin B12 343pg/l, Folic acid 4.ng/l, Reticulocyte count 20%, Haptoglobulin 2, Direct and indirect Coombs’ test was positive. Bone marrow aspiration and biopsy was completely normal. A diagnosis of idiopathic AIHA was made. Prednisolone 1mg/kg and folic acid 5mg was administered daily and the patient was discharged on tapering doses of prednisolone. Biopsy of an axiller lymph node was performed as a diagnostic procedure, and it was reported as Nodular sclerosing Hodgkin’s disease. Medium-power view of the lesion shows an organoid with small rounded nests of tumor cells surrounded by thin fibrous septae (hematoxylin and eosin, ×100) (Figure 1).
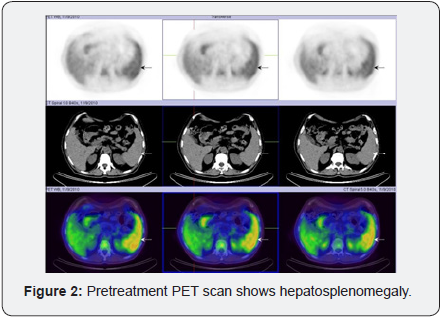
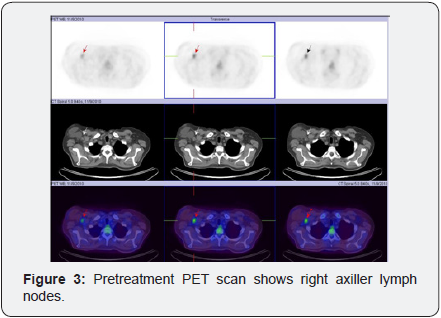
On PET scan was hepatosplenomegaly and right axiller lymph nodes (Figure 2 & 3). This was consistent with a diagnosis of stage I B HD spleen involment. Subsequently the patient received 4 cycles of adriamycin, bleomycin, vinblastine and dacarbazine (ABVD) chemotherapy and 30Gy radiotherapy on his right axiller area.
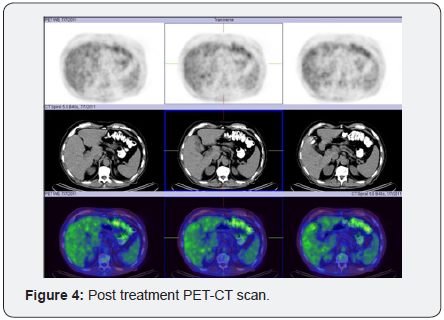
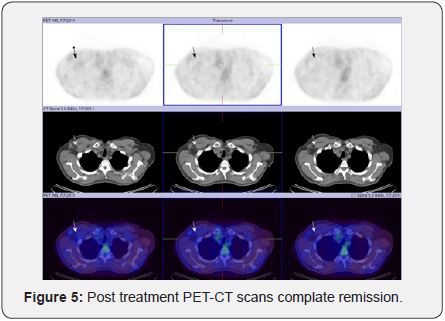
Post treatment PET-CT scans showed complete resolution of the disease (Figure 4 & 5). Repeat hemoglobin, red blood cells indices and peripheral blood smear were all normal. Markers of hemolysis indicated remission of AIHA.
Discussion
AIHA is a recognized complication of lymphoproliferative disorders, especially chronic lymphocytic leukemia. HD, however, is rarely associated with AIHA. This association was first described by Eisner et al. [4]. The reported frequency of Coombs’ positive hemolytic anemia in adults with HD has ranged from 0.2 percent in a large series of 492 patients from Europe to 3 and 4 percent in two American studies [1,4-6]. These figures show that AIHA in HD is an uncommon association. When HD is accompanied by AIHA, the hemolysis is usually detected at the time of diagnosis or a relapse [6]. Very rarely has it been reported to precede the diagnosis of HD, in one case by up to 7 years [1,7,8]. İmmune-mediated hemolytic anemia is mostly seen in the nodular sclerosing subtype and in mixed cellularity subtypes, as in this case. The exact mechanism of AIHA in HD is still not clear. However it may be postulated that the autoantibodies are directly produced by tumour cells or are related to an immune regulatory phenomenon. It is possible that there is an autoimmune process at the early stages of HD in which antibodies are produced against the tumour as well as the red blood cells as a para-neoplastic phenomenon. The antibodies prevent the growth of the tumour at least initially, which later escapes the anti tumour effect of the antibodies and finally manifests as HD. Although the specificity was not determined in our patient, the antibody associated with AIHA in some patients with HD has been identified as an anti transition (It) antibody [9]. Patients with HD are known to have an impaired cell mediated immune response due to decrease in number as well as function of T lymphocytes. Decreased number of cytotoxic T cells could lead to excessive autoantibody production. This appears to be partly due to hyperactivation of B-cells. This concept is further strengthened by reports of high incidence of AIHA following T-cell depleted allogeneic bone marrow (BM) or peripheral blood stem cell (PBST) transplantation [10]. Treatment with anti CD20 antibody rituximab, which suppresses the B-lymphocytes, has shown to be effective in idiopathic AIHA as well as for immune haemolysis associated with BM or PBST transplantation [11,12]. Acquired AIHA has been described to be associated with an underlying disease in more than fifty percent of cases. Many patients with apparent idiopathic AIHA eventually manifest the presence of an associated disease [1]. HD is one of the conditions to be considered in the presence of warm agglutinin haemolytic anemia. Although the initial treatment of AIHA is steroids, immune hemolysis associated with HD requires definitive treatment with systemic chemotherapy. Administration of steroids probably altered the course of the disease and made the diagnosis of HD difficult and late to establish. Some patients with AIHA may have a minimal tumour burden initially and the diagnosis of HD may be easily missed [1,2].
Conclusion
This case shows that that patients with AIHA should be regularly and carefully monitored, clinicians should be aware of the possibility of immune hemolytic anemia in patients with Hodgkin’s disease presenting with anemia, and distinguish it from the anemia of chronic disease.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment