Juniper Publishers- Open Access Journal of Case Studies
Symptomatic Pulmonary Embolism after Achilles Tendon Repair
Authored by Naoki Yoshida
Abstract
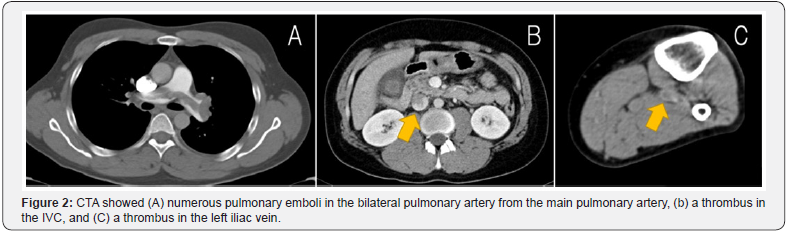
The incidence of symptomatic pulmonary embolism (PE) following treatment for Achilles tendon rupture is rare. Here we present a case of a 40-year-old man with symptomatic PE, who was operated 24 days ago for Achilles tendon rupture. Computed tomography angiography (CTA) showed numerous pulmonary emboli in the bilateral pulmonary artery from the main pulmonary artery and a thrombus in the inferior vena cava (IVC) from the left iliac vein. The patient was treated using an anticoagulant and IVC filter and showed a good functional outcome at the five-month follow-up. It is important to examine and treat Achilles tendon rupture, keeping in mind PE.
Background
Achilles tendon rupture is common in orthopedic practice [1]. In both operative and conservative treatments, cast immobilization is necessary to protect the repaired tendon [2]. There are a few reports on the incidence of symptomatic PE following treatment for Achilles tendon rupture [3,4]. This current report underscores the possibility of acute PE in cases of Achilles tendon rupture.
Case Presentatıon
A 40-year-old man presented to the emergency department with a painful left heel. The pain was suddenly brought on during aerobics, but he was able to walk despite the pain. He had no past medical history and was not on any medication at that time. On physical examination, there were a palpable gap in the left Achilles tendon, and Thompson test was positive. We diagnosed left Achilles tendon rupture and discussed the treatment with the patient. He agreed to have surgical repair and was operated upon nine days post injury. The tendon was sutured using the Kessler technique (Figure 1) and was subsequently protected by a below-the-knee cast in a plantar-flexed position. The patient was permitted to walk on crutches. He was discharged from our hospital, and he returned to work with no complications.

Two weeks postoperatively, his cast was converted into an Achilles tendonitis brace. However, 24 days postoperatively, he presented to the emergency department with sudden severe dyspnea. On examination, his blood pressure was 88/59mmHg, pulse 98/min, and respiratory rate 26/min, with an O2 saturation of 93% in room air. CTA showed numerous pulmonary emboli in the bilateral pulmonary artery from the main pulmonary artery (Figure 2A). CTA also showed a vein thrombus in the IVC (Figure 2B) from the left iliac vein (Figure 2C). There was no thrombus in the right iliac vein. The patient was administered an anticoagulant and IVC filter as treatment for acute PE. The side of the Achilles tendon surgery coinciding with the side of the thrombus strongly suggested the Achilles tendon repair was the cause of PE. One month later, angioplasty revealed the thrombus had disappeared, so the IVC filter was removed. The patient showed a good functional outcome and returned to work at the six-month follow-up.
Discussion
The Achilles tendon is the largest tendon in the body, but it often ruptures, mostly during sports activities [5]. Injury is caused by a sudden pushing off from the weight-bearing forefoot with the knee in extension, unexpected ankle dorsiflexion, and violent dorsiflexion of a plantar-flexed foot [6]. Achilles tendon rupture can be managed by both operative and nonoperative strategies. It is generally accepted that surgery should be performed for athletes and young and fit patients and that conservative treatment may be suitable for the elderly [7]. Both treatments include a period of immobilization, which is a welldocumented risk factor for deep vein thrombosis (DVT) [2]. In the current literature, the reported incidence of DVT after Achilles tendon rupture is highly variable, ranging from less than 1% to 34% [8]. Common symptoms and signs of DVT are unilateral or asymmetric swelling, leg edema, pain, erythema, fever, and leg warmth [9]. Actually, most DVT patients are asymptomatic, and only 9%–17% of them show clinical manifestation [9]. However, silent DVT can progress to a PE, a significant source of mortality [10].
There are several controversies surrounding thromboprophylaxis for Achilles tendon rupture. Several authors have recommended that the use of milder forms of prophylaxis, such as aspirin, also be explored [11]. Others have recommended that prophylactic anticoagulation not be routinely administered [12]. It is important to examine and treat Achilles tendon rupture, keeping in mind DVT and PE.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment