Juniper Publishers- Open Access Journal of Case Studies
Cerebral Mucormycosis Mimicking a Brain Tumor
Authored by Yin Liu
Abstract
We describe a case of intracranial mucormycosis in an immunocompetent child with perfusion features mimicking a brain tumor. Saksenaea species has previously been reported in immunocompetent patients. The source of the infection in our patient was unknown. On brain MRI, the unusual curvilinear and nodular enhancement pattern may reflect the angioinvasive nature of the organism, not previously reported. The finding of increased CBV is typically associated with neoplasms, with CNS infections typically demonstrating decreased CBV. This case demonstrates that fungal infection may present with increased CBV.
Keywords: Mucormycosis; Cerebral; MRI perfusion; Increased cerebral blood flow; Brain tumor
Abbrevations: MS: Multiple Sclerosis; PWI: Perfusion-Weighted Imaging; DWI: Diffusion-Weighted Imaging; CBV: Cerebral Blood Volume; CNS: Central Nervous System; ROCM: Rhino-Orbital-Cerebral Mucormycosis
Case Report
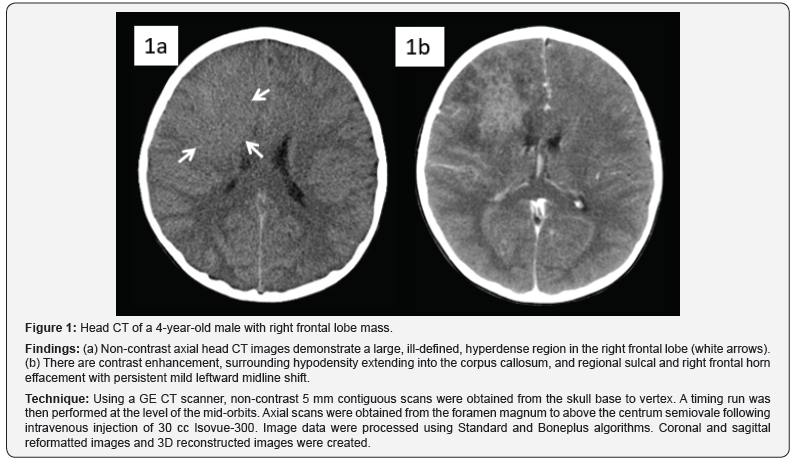
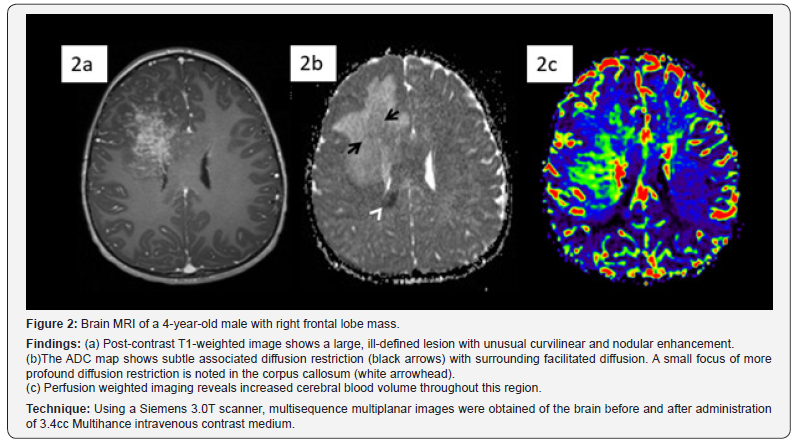
4-year-old healthy male presented to the emergency room with intractable vomiting, worsening right frontal headaches for one month, and drowsiness for one day. Head CT demonstrated an ill-defined hyperdense right frontal lobe lesion (Figure 1). MRI showed an irregularly enhancing right frontal lobe lesion which extended to the corpus callosum. Subtle associated diffusion restriction was noted with increased cerebral blood volume (Figure 2). A high-grade, hypercellular tumor was suspected, although the enhancement pattern was unusual. A generous brain biopsy was performed with intraoperative pathology revealing granulomatous fungal encephalitis and the lesion was grossly illdefined. Tissue culture confirmed growth of Saksenaea species.
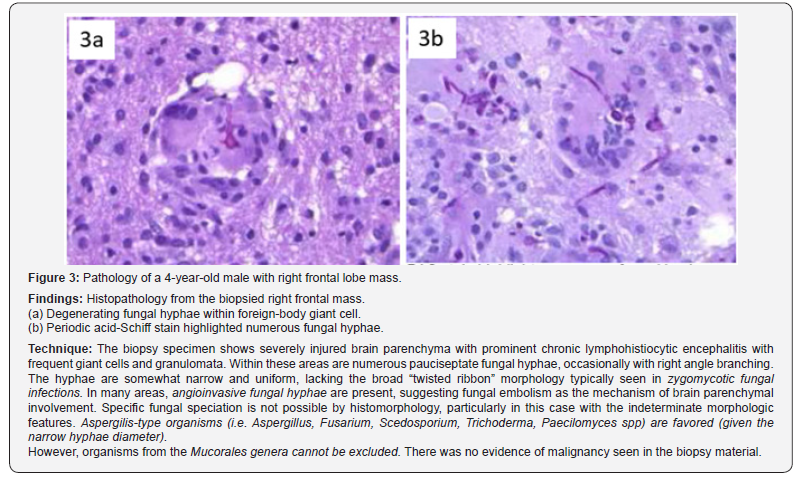
Extended work up ruled out diabetes, immunodeficiency, and disseminated systemic fungal infection, including blood work for congenital or acquired immunodeficiencies (serum immunoglobulins for humoral deficiency, lymphocyte subsets for cellular deficiency, and CH50 for complement deficiency, oxidative burst for chronic granulomatous disease, Quantiferon Gold for TB, and HIV), a chest CT for fungal respiratory infection, an echocardiogram, a complete ophthalmic exam, and gastric endoscopy. He completed a course of daily IV liposomal amphotericin B 10mg/kg for 14 weeks and is currently on the same daily total dose but three times weekly. The plan is to continue antifungal medications for a minimum of 12 months. He has also been on posaconazole IV (dose adjusted per serum trough) and terbinafine 6.5mg/kg/day enterally. He also received hyperbaric therapy for 14 treatments (Figure 3).
He has spent the past 6 months in the hospital. Despite poor prognosis, parents have chosen for him to receive full treatment. He is now status post decompressive hemicraniectomy secondary to refractory intracranial hypertension, in a minimally conscious state, dependent on gastrostomy feeding and a tracheostomy tube without mechanical ventilation. He has severe spasticity and paroxysmal sympathetic hyperactivity, which are treated with medications (clonidine, diazepam, baclofen and dantrolene), physical, and occupational therapies.
Discussion
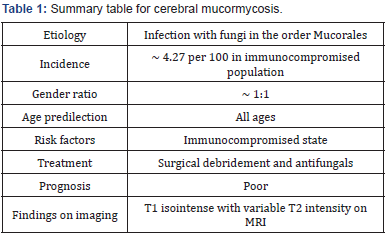
Etiology & demographics
Rhinocerebral mucormycosis is a rare opportunistic infection of the sinuses, nasal passages, oral cavity, and brain caused by saprophytic fungi. Rhino-orbital-cerebral mucormycosis (ROCM) is a life-threatening rare, opportunistic, and severe angioinvasive infection, which is typically seen in patients with severe immunodeficiencies such as hematological malignancies undergoing chemotherapy, or in diabetic patients [1,2]. However, Saksenaea species in the order Mucorales has previously been reported in immunocompetent patients [3].
Clinical & imaging findings
Based on anatomic localization, mucormycosis can be classified as 1 of 6 forms:
a) Rhinocerebral,
b) Pulmonary,
c) Cutaneous,
d) Gastrointestinal,
e) Disseminated, and
f) Uncommon presentations [2].
Manifestations of mucormycosis depend on the location of involvement. Central nervous system (CNS) disease manifests as headache, decreasing level of consciousness, and focal neurologic symptoms/signs including cranial nerve deficits. Patients with CNS involvement may have a history of open head trauma, intravenous drug use, or malignancy. Here we discuss an unusual case of intracranial mucormycosis, presenting in an immunocompetent patient as an intracranial mass lesion. The source of the infection in our patient is unknown.
Brain lesions are typically T1 isointense with variable T2 intensity on MRI [4]. MRI signal intensity of mucormycosis lesions tends to be isointense or hypointense in all sequences. After the administration of gadolinium, the lesions typically have variable enhancement patterns (ranging from homogeneous to heterogeneous or no enhancement) [4]. Diffusion weighted imaging typically shows markedly reduced diffusion [5]. The unusual curvilinear and nodular enhancement pattern in our case may reflect the angioinvasive nature of the organism, not previously reported. The finding of increased cerebral blood volume (CBV) is typically associated with neoplasms, with CNS infections typically demonstrating decreased CBV [6]. This case demonstrates that fungal infection may present with increased CBV.
Treatment & prognosis
Current guidelines on treatment of ROCM include prompt initiation of liposomal amphotericin B therapy and complete surgical resection, when possible [7]. Adjunctive therapies such as hyperbaric oxygen, colony-stimulating factors, and iron chelators are all controversial. Mycormycosis is one of the rapidly progressing and lethal form of fungal infection. Risk factors include diabetes and neutropenia [8]. The underlying conditions can influence clinical presentation and often delay diagnosis, with resultant poor outcomes [9]. Patients with rhinoceerbral mycormycosis spreading outside the sinonasal cavity have a poor prognosis despite aggressive surgical debridement and medical management [10] (Table 1).
Differential diagnoses
Tumor: A tumor is suspected when a focal density or signal alteration is seen displacing or infiltrating adjacent structures with or without a matching contrast enhancement and possibly surrounded by vasogenic edema. High grade tumors typically show increased CBV.
Abscess: the classic tumor-like lesion is an intracranial abscess [11]. Most intracranial abscesses are bacterial (staphylococcus, streptococcus, and pneumococcus). Intracranial abscesses may present with imaging features that are identical to high-grade neoplasms. Abscesses are round, mass lesions with various degrees of adjacent vasogenic white matter edema and a strong peripheral contrast enhancement. The ring of enhancement is usually closed and may appear thicker towards the direction of the cortex. The pus within the abscess typically showed a restricted diffusion on diffusion-weighted imaging (DWI), whereas necrosis in the center of malignant tumors typically shows an increased diffusion.
Subacute ischemia: These lesions may have a significant mass effect with irregular contrast enhancement. The clinical history with acute onset of symptoms and a matching clinical history can assist with differential. Most lesions are located within a vascular territory with simultaneous involvement of cortex and adjacent white matter. Anatomic MRI shows restricted diffusion on DWI and hypoperfusion on perfusion-weighted imaging (PWI). Demyelination: Various demyelinating diseases, including tumerfactive multiple sclerosis (MS), acute disseminated encephalomyelitis, and progressive multifocal leukoencephalopathy may present tumor-like. Typically, MS plaques show an incomplete ring of contrast enhancement towards the cortex. Advanced imaging can be helpful for diagnosis, including DWI, MRS and PWI. Tumefactive plaque typically shows marginal diffusion restriction and an aggressive spectroscopic profile with increased choline, decreased NAA and presence of lactate. CBV would typically be decreased. A rapid response of the lesion to corticosteroid treatment is suggestive of demyelinating disease. Tumors and abscesses do not respond quickly (Table 2).
.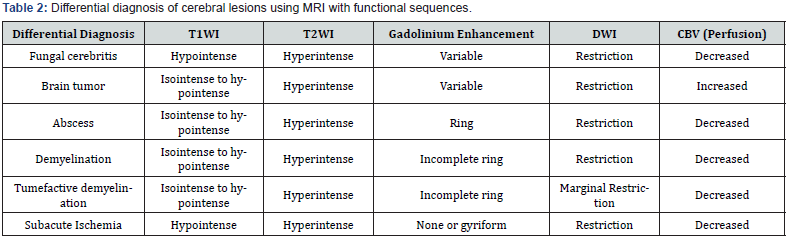
MRI = Magnetic Resonance Imaging
T1WI = T1-weighted MRI turbo sin echo sequence
T2WI = T2-weighted MRI turbo spin echo sequence
DWI = Diffusion weighted imaging
CBV = Cerebral Blood Volume.
Teaching Point
Intracranial mucormycosis in an immunocompetent child may present with perfusion features mimicking a brain tumor. Fungal infection may present with increased CBV.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment