Juniper Publishers- Open Access Journal of Case Studies
Osteopetrorickets - A Paradoxical Association between Osteopetrosis and Rickets - A Rare Case Report
Authored by Madhan Jeyaraman
Abstract
Background: Osteopetrosis is a rare autosomal recessive disorder, characterized by failure of osteoclasts to resorb bone leading to impairment of bone modelling and remodelling. The defect in bone turnover results in skeletal fragility despite increased bone mass. Despite high positive total body calcium balance, rickets arises when the serum calcium-phosphorus product is insufficient to mineralize newly formed Chondroid and Osteoid. When both these conditions are seen in the same patient, it is called ‘Osteopetrorickets’, a paradoxical association.
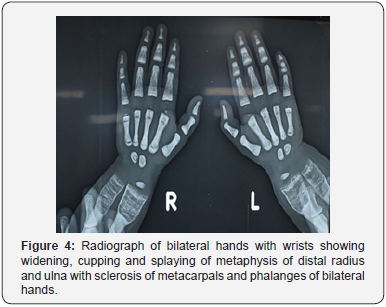
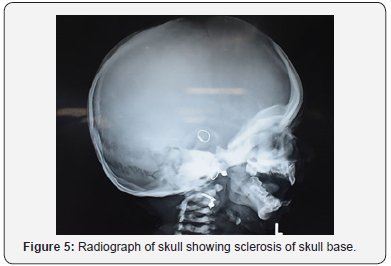
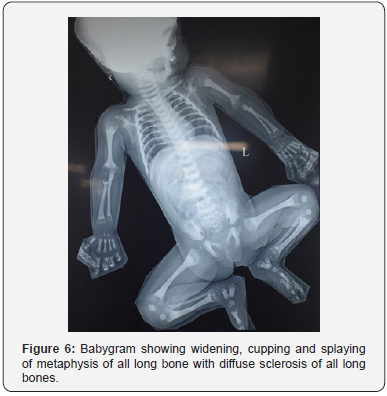
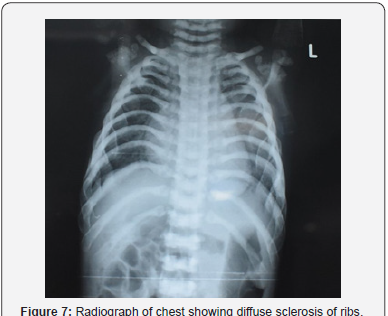
Case report: A 2 years 5months old female child presented with h/o inability to walk and bear weight and recurrent respiratory tract infections. The child was anaemic, with prominent ricketic features. On systemic examination, the patient had hepatosplenomegaly. Laboratory investigations showed severe anaemia, thrombocytopenia, hypocalcemia, hypophosphatemia, decreased Vit D3 and elevated serum PTH & serum alkaline phosphatase levels. The skeletal survey revealed features of rickets, sclerosis of skull and long bones, and bone in bone appearance. Fundus examination showed B/L optic atrophy. Otological examination BERA showed B/L sensorineural hearing loss. CT scan of long bones showed diffuse cortical sclerosis of all long bones.
Discussion: Malignant infantile osteopetrorickets is a rare paradoxical association. The diagnosis of the condition is by regular biochemical and sradiological investigations. Here the patient showed improvement with supplemental calcium, calcitriol and blood transfusion. Definitive treatment is HLA identical bone marrow transplantation. Death usually occurs in early childhood due to bleeding, anaemia and infections.
Conclusion: Early diagnosis and treatment should be instituted for patients with high index of suspicion with ricketic features and prompt genetic counselling has to be done regarding the nature of inheritance pattern of diseases.
Keywords: Osteopetrorickets; Autosomal recessive; Calcitriol; Bone marrow transplantation
Introduction
Malignant infantile osteopetrosis is an autosomal recessive and a rare congenital disorder of bone resorption. The genetic defect is due to the mutations in the gene coding for an osteoclast specific vacuolar pump (TCIRG1 subunit) [1]. Despite the failure of osteoclasts to resorb immature bone, the formation of abnormal cavity in the bone ensues. Pathologically, there is a persistence of the primary spongiosa characterised by cores of calcified cartilage within bone. Abnormal remodelling of primary, woven bone results in “brittle” bone which is prone to fracture [2]. The co-existence of features of osteopetrosis and rickets in a same individual result in a paradoxical condition called Osteopetrorickets [2,3]. Here in this article, we have reported a case with classical features of osteopetrorickets and its management.
Case Report
A 2 years 5months old female child brought by mother born to first issue of second-degree consanguineous couple delivered by birth natural presented with h/o inability to walk and bear weight and recurrent respiratory tract infections. This child was born to a consanguineously married couple. The child had global developmental delay with an IQ of 50. The child was short, with height of 94cm and weight 13kg, which were <5 centile on NCHS charts. On head to toe examination, the patient was anaemic, with prominent eyes, frontal and parietal bossing, short trunk dwarfism, craniotabes, pectus excavatum, costochondral beading, widening and broadening of wrists, bowed knees and double malleoli (as shown in figure 1-3).
On systemic examination, the patient had hepatosplenomegaly without any significant cardiac and neurological manifestations.
The patient was evaluated for further which revealed the following findings:
a) Hematological investigations showed severe anaemia (Hb - 2.9g%) and thrombocytopenia (Platelet 0.68L/cu mm)
b) Biochemical investigations showed hypocalcemia (7.6mg/dL), hypophosphatemia (2.3mg/dL), Vit D3 - 4.54ng/ml, serum PTH - 72.5pg/ml and serum alkaline phosphatase - 759IU/
c) Skeletal survey revealed diffuse metaphyseal widening with cupping of metaphysis, sclerosis of skull and long bones, and bone in bone appearance (Figure 4-7).
d) Fundus examination showed B/L optic atrophy.
e) Otological examination BERA showed B/L sensorineural hearing loss.
f) CT scan of long bones showed diffuse cortical sclerosis of all long bones.
The patient was treated conservatively who showed a significant improvement with supplemental syrup calcium 500mg twice daily for 6 months and high dose calcitriol 6,00,000U once intramuscular injection followed by daily 6000 units oral for 4 weeks and tapered to 400 units per day for 6 months. The patient received 6 pints of packed red blood cell transfusion. The patient was subjected for serum calcium, phosphorus, alkaline phosphatase and PTH levels every month and radiological analysis once in 2 months. The patient was followed up every month for 6 months and 6th monthly interval for 2 years which showed improvement in the general condition of the patient.
Discussion
Malignant infantile osteopetrosis is a rare autosomal recessive disorder of osteoclast function characterized by abnormally dense bone and failure of resorption of calcified cartilage which leads to impaired bone modelling and remodelling. In this condition, despite high calcium balance, there is a failure of mineralization of chondroid and osteoid results in rickets. When both these conditions are seen in the same patient, it is called ‘Osteopetrorickets’, a paradoxical association [2,3].
The genetic defect is due to the mutations in the gene coding for an osteoclast specific vacuolar pump (TCIRG1 subunit) [1]. The presence of rickets worsens the symptoms of osteopetrosis. Rickets is associated with increased lethargy, irritability, poor feeding, growth retardation and pathological fractures, and hence the patient needs effective treatment. In osteopetrosis, the patients are often advised to reduce calcium intake and the osteoclasts do not respond to PTH which is responsible for maintaining calcium balance lies on the kidneys and intestine. Patients on limited calcium intake and poor intestinal absorption due to prednisolone, which is the reason for hypocalcemia and hypophosphatemia. Persistence of hypocalcemia and hypophosphatemia results in inability to mineralize the newly formed chondroid and osteoid and hence the paradoxical association of rickets and osteopetrosis results.
The criteria to diagnose Osteopetrorickets are as follows [2-4]
a) Recurrent infections
b) Presence of ophthalmic and ontological affection such as optic atrophy and sensorineural hearing loss
c) Clinical features of rickets: Frontal bossing, Harrison sulcus, pectus carinatum, genu varum/valgum, double malleoli
d) Biochemical investigations: Hypocalcemia and hypophosphatemia with elevated serum alkaline phosphatase and serum PTH levels.
e) Radiological features: Widening, cupping and splaying of metaphysis of long bones and diffuse sclerosis of long bones
The presence of all 5 criteria mandates to label the condition as osteopetrorickets.
The available treatment options include HLA identical bone marrow transplantation, glucocorticoid therapy, use of large doses of calcitriol and calcium [5-7]. Usually death ensues in view of anemia, bleeding and recurrent infections.
We treated our patient using high dose calcitriol and calcium along with six pints of packed red blood cell transfusions. The patient was subjected for serum calcium, phosphorus, alkaline phosphatase and PTH levels every month and radiological analysis once in 2 months. The patient has been subjected for multidisciplinary follow up for every month for 6 months and 6th monthly interval for 2 years which showed improvement in the general condition of the patient. Further follow up of the patient has to be done annually till the skeletal maturity.
Conclusion
A paradoxical condition, Osteopetrorickets, to be diagnosed early and prompt management has to be instituted to prevent further complications and death. The natural history and clinical course of the disease has been explained to the parents and genetic counselling has been given for future pregnancies. Due to lack of facilities, the genetic work up for the patient and the parents have been declined.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment