Juniper Publishers- Open Access Journal of Case Studies
Lipografting - and Sculpturing in Female-to-Male Transgender Patients
Authored by Delia L Francia
Abstract
This case report presents several surgical procedures that amply lipotransfer and -sculpturing to treat specific volume sequelae and scar-related impairments in FtM patients after failure of conservative surgical primary therapy. From November 2016 till November 2018 three FtM patients with typical scar related sequelae underwent sequential lipografting – and sculpturing. Our minimally invasive operative protocol (ACRT) was combined if required to a gender reassigning liposculpturing of the trunk or forearm augmentation for flap preformation. Clinical and aesthetic outcome were measured with photographs, the Patient and Observer Scar Assessment Scale (POSAS), Visual Analogue Scale (VAS) for pain, ROM measurements and nerve conduction studies (NCS). In all three patients a relevant functional and aesthetic improvement was achieved associated with very short hospitalization (average 3.2 days) and minor complications like swelling or bruising of the donor site. Clinical outcome showed improved scar appearance; 55% mean decrease of pain perception leading to 37% higher ROM in the left wrist mostly in extension. Increase of neophallus’ size or forearm’s subcutaneous layer prior to phalloplasty as well as a typical V-shape masculine trunk were accomplished after maximum three procedures.
Keywords: Liposculpturing; Fat grafting; Transgender surgery; Scar therapy
Abbrevations: FtM: Female to Male; ACRT: Adipose Cells Derived Regenerative Therapy; POSAS: Patient and Observer Scale; VAS: Visual Analogue Scale for pain; ROM; Range of Joint’s Motion in Degrees; NCS: Nerve Conductive Studies /Measurement for Electrophysiological Functionality
Introduction
Lipografting is emerging as a treatment for postoperative sequelae, namely postoperative or posttraumatic contour and volume defects as well as dermal scars [1,2]. Liposuction may serve to remove excess volume, whereas lipografting of the harvested adipose tissue can be used to enhance and restore soft tissue volume defect [3-6]. Furthermore, lipografts remodel scar tissue by unknown mechanisms, which improves the elasticity and aesthetic aspect of the skin [7]. Another important feature of lipografting is pain reduction in neuropathic scars [8,9].
A group that could benefit from lipografting as a reconstructive treatment option for postoperative sequelae are patients suffering from gender identity disorder, that opt to undergo or underwent female-to-male (FtM) sex reassignment surgery. The term gender identity disorder is used for individuals, who experience a strong and persistent cross-gender identification and a persistent discomfort with their anatomical sex, as manifested by a preoccupation with getting rid of one’s sex characteristics or the belief of being born with the wrong sex [10]. It is a relatively rare condition, with a prevalence roughly estimated from 1:30,040 to 1:104,000 in assigned females [11]. However, the prevalence of operative male-to-female transition is four times higher compared to female-to-male. Traditionally, the process of FtM transition is a staged. Initially, hormone therapy with testosterone is started to induce virilisation [12]. Then, the first stage of surgical sex reassignment is usually a subcutaneous mastectomy, which may be combined with hysterectomy and bilateral salpingo-oophorectomy. The second stage involves phalloplasty or metoidioplasty, combined with scrotoplasty and eventually with vaginectomy [13,14]. Although several techniques for phalloplasty e.g. anterior thigh flap, suprabubic flap, lattissimus dorsi flap are described the literature, the radial forearm flap phalloplasty is the most frequently performed [15]. After successful microsurgical transplantation a penile prosthesis, i.e. an inflatable erection device, and testicular prosthesis can be implanted [16].
The main functional and aesthetic aims of FtM sex reassignment surgery are micturition in standing position, visible bulk in under- or swimwear and preservation of genital sensation combined with the ability to achieve erection and penetration. These goals should be implemented in the therapeutic concept by surgeons, providing transmen an optimal fit in the desired gender role. However, sex reassignment surgery is linked to a high complication rate, while FtM patients also require numerous operative revisions to improve functional and aesthetic outcome [17]. Currently, no specific reconstructive treatment has evolved or particularly declared to improve the radial flap donor-site disfigurement, as well as functional impairment, i.e. in range of motion (ROM), due to the lacking subcutaneous adipose layer [18,19]. Furthermore, difficult-to-treat problems in FtM patients are painful and disfiguring scars on several body parts e.g. the pectoral or inguinal region. Genital skin irritation or pressure sores occur due to insufficient prosthesis coverage (i.e. penile or testicular implants) and frequent soft tissue volume defects (e.g. disproportionate scrotal or penile size) [20,21]. A remaining female aspect of the whole trunk including a wide hip region even after standardized mastectomy and hormone therapy may cause persistent discomfort and has not been described in a selective plastic surgical procedure yet [22]. Hence literature lacks standard operating protocols concerning sequelae after radial forearm flap phalloplasty or unsatisfactory results due to penile reconstruction [23-25].
This report describes results of specific designed operative concepts in order to approach the aforementioned problems as indications to revision systematically e.g. by using our minimal invasive scar release concept called Adipose Cells derived Regenerative Therapy (ACRT) in typical scar regions [26]. The pectoral contours were enhanced by lipografting and combined to liposculpturing of the lateral flanks and abdominal part for utter masculinization of the trunk. FtM patients in different stages of their gender affirmation process were included and treated because of refractory symptoms or impairments after mastectomy, free radial forearm flap phalloplasty after total failure of conservative therapy. Clinical outcomes were measured after at least three months follow-up period in order to assess efficacy with a low complication rate.
Material and Methods
Refractory painful scar adhesions, disfiguring trunk/hip parts, poor penile size or prosthesis coverage were treated in 3 female-to-male transgender patients from 2016 to 2018. Each patient underwent 3 operative procedures (P1-3) and these cases were retrospectively reviewed (Table 1). Previously to operation patients received at least one year of conservative scar therapy i.e. massages, silicone gel, compression, intensive occupational or pharmacologic therapy. But despite these interventions all major symptoms persisted, i.e. scar contraction leading to an obstructive sensation of the forearm with decreased mobility of the wrist, allodynia, conspicuity of the trunk and neophallus aggravating stigmatization or persistent genital skin problems due to insufficient tissue coverage of the penile prosthesis. Ultimately, we addressed the phenomenon of decreased penile size due soft tissue shrinking after phalloplasty in two patients – on the one hand with engraftment of the neophallus and on the other with preformation of the forearm through lipografting before radial free flap transplantation. These indications had been listed for our investigation and to minimize treatment related bias, all operations were done by the same senior surgeon to minimize bias of surgery in post-op evaluations. The research was conducted in agreement with the ethical rules for human experimentation as stated in the Declaration of Helsinki. Demographical and clinical data regarding scar characteristics, perception of pain, range of motion were kept prospectively as a part of a research on lipografting on scars, approved by the internal Medical Ethical Committee (METC 167/2015MPG43). All patients gave written informed consent after being informed about the procedure and its consequences.
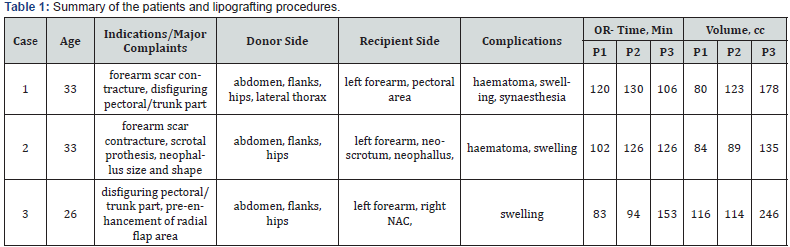
OR-Time = Operation -Time, min = minutes ; P = Procedure.
Surgical Techniques
Patients presenting with either radial flap donor site scars or pectoral scars after mastectomy, were treated according to our standardized minimal invasive scar release procedure called the ACRT protocol [26]. In brief, the scar tissue of at the radial flap donor site or on other body parts was loosened by means of a minimal invasive scar release technique through maximum two stab incisions. Intra- and subdermal fibrotic tissue was undermined strictly horizontally to the skin level with specific sharp needles of different diameters (16 to 22 Gauge). Each scar area (15 to 80cm2) had to be individually prepared for the grafting of lipoaspirates by following the projected spider web like design. The lipograft was harvested from the abdominal and hip region using the body-jet system with modified Klein’s tumescence solution for waterjet assisted liposuction (human med AG, Schwerin) [27]. The liquid consists of isotonic saline solution supplemented with epinephrine (final dilution 0,0001%, Infectopharm), Xylocaïn (0.049%, Astrazeneca GmbH) and sodium bicarbonate (1.48%, Fresenius Kabi Deutschland GmbH). While waterjet assisted harvesting, the lipograft was contemporarily washed and filtered through the Lipocollector III°- System (human med AG, Schwerin). Portions of 50cc were decanted and after 7min transferred to 10cc Luer-Lock syringes. Fat was re-injected intra - and subdermally into the pre-treated scar area with a 7 to 12cm long blunt tip cannula. Stab incisions were closed by temporary single sutures and dressing.
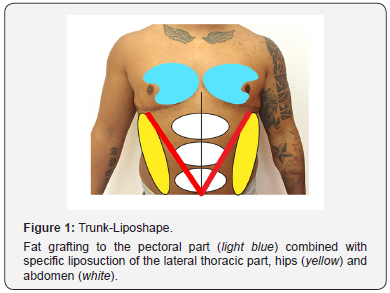
In order to gain a more masculine aspect of the chest wall and the abdominal part, we planned and marked the different areas of the trunk to address (Figure 1). By using a 3.8mm sized multiple-hole cannula and water jet assisted liposuction the determined refinement of the hip and lateral thoracic part was performed in the first place. Preparation of the lipograft occurred with the Lipocollector III°- System and the adipose tissue was prepare in 10cc Luer –Lock syringes ready for reinjection. One stab incision was placed on each side in the lower margin of the NAC. Subdermal and intramuscular lipotransfer took place with 7 to 12cm long blunt tip cannulas. In this way the inner and lower margins of the pectoral muscle were enhanced and underlined the masculine pectoral contours. Intraoperative the patients were sat in an upright position in order to control stepwise the symmetry and bilateral engraftment. The selective liposuction of excess fat on the abdomen, hips and flanks generally lead to the characteristic V-shape of a masculine trunk. Stab incisions were closed with single prolene sutures and covered with sterile dressings. The grafted area was cushioned with soft cotton bandings and a tight-fitting compression garment was put on in the operating room. Postoperatively, all patients received antibiotic treatment with cefuroxime 500mg per OS three times daily for a total of 5 days. A cushioned dressing was applied to the recipient site in order to avoid pressure on the lipograft for at least 10 days. In case of radial flap donor site augmentation, splinting was used for five days to avoid muscular tension or shear forces on the lipograft. Temporary sutures were removed after 5 to 7 days during routine control. Compression on the lipograft donor site was carried out for at least 4 weeks and muscular stress or sports were only allowed afterwards. Followup controls took place after one week, one and three months postoperatively.
Results
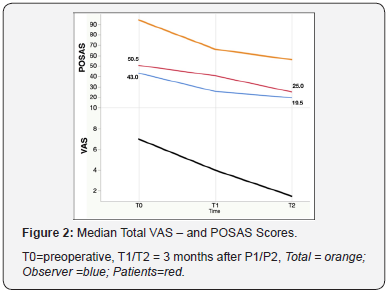
Almost all nine interventions contained at least two surgical techniques e.g. trunk liposhape combined with ACRT on several body parts with a median operation time of 120min (range 83 to 153min). On average 129cc of lipograft (range 80 to 246cc) was used per procedure with a total mean volume of 735cc per patient. For the trunk liposhape 160 to 200cc was needed and a total of 205cc was inserted for penile and scrotal correction. We recorded no major complications, but two minor complications in nine interventions due to our operative techniques. The first complication consisted of allodynia in the form of an electrical sensation and numbness in the first three fingers after lipografting in the radial flap donor site, indicating compression of the carpal tunnel. These symptoms were managed with conservative treatment and subsided spontaneously after five days. The second minor complication was haematoma formation after liposuction, which was treated conservatively and subsided after two weeks. Of note, none of the patients developed infection, donor-site irregularity, reactive scaring, oil cysts, fatty clumps or showed insufficient reuptake. Scars related issues and painful impairments were objectified by questionnaires (POSAS, VAS) preoperatively and 3 months after P1 and P2 (Figure 2). Benefit resulted by a notable reduction of the total scores for patients (50.5/25.0) and for observers (43.0/19.5) respectively. VAS also reduced, indicating a relief of pain due to the procedures applied. Preoperatively measured ROM and Tinel signs on the forearm improved mean 36.5% mostly in extension and radial abduction after the sequential subscar fat injection.
Case Reports
Case 1

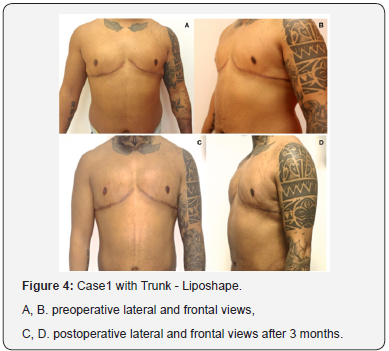
33 years old non-smoker with a BMI 28.4kg/m2, was enrolled in November 2015 for a painful scar adherence on the donor site two years after free radial forearm flap transplantation. He presented a skin type V according to Fitzpatrick with hypertrophic scarring and high pigmentation also on the pectoral area. Full skin graft originated from the inguinal area presented severe scar contraction on the left forearm and led to lessened movements such as 40°extension, 10°radial and 25°ulnar abduction in the wrist. The patient complained about an obstructive sensation due to the reduced circumference on the proximal and distal edges of the scar area (Figure 3A). A Tinel sign was detected 1.7cm distal and 3 cm proximally the superficial radial nerve area. Hypersensitivity led to a reduced quality life, e.g. the disability of wearing long arm clothes. Prior conservative treatment with silicone gels and sheets, compression garments and massages failed to alleviate patient’s complaints. Besides overweight and conspicuous scar formation brought to an unpleasant aspect of the trunk and pectoral area (Figure 4A & 4A). We performed three sessions of minimal invasive scar release method to the forearm and with 80cc, 123 cc and 20cc of fat graft. After the first 3 months follow up the patient already gained 5° to 10° in the ROM of the wrist joint. Tinel sign was decreased detectable 1cm distal and 1.6cm proximally the radial nerve area, indicating a local cushioning or embedding effect of the inserted lipograft. After the next intervention functional impairments like neuropathic pain diminished even more. This was confirmed by reduced VAS scores from preoperatively 6 (nearly acceptable pain) to final 1 (almost none). Finally, the initial tethering scar aspect in texture regained high pliability and ROM in the donor wrist improved to painless completion (Figure 3B). By using the aforementioned trunk liposhape approach, we removed 390cc pure fat and transplanted 160cc graft volume in the predefined parts. In this way we obtained a dominant masculine aspect of the pectoral contours combined with a flattening definition of the lateral thoracic part, flanks, abdomen and hips (Figure 4C & 4D).
Case 2
33 years old non-smoker with a BMI 20.5kg/m2, showed in January 2016 painful and hypersensitive scar formation after free radial forearm phalloplasty with full split skin graft to the donor site in October 2012. ROM was reduced with 25°extension, 10°radial and 15°ulnar abduction. In addition, recurrent wounds and skin lesions occurred due to poor skin coverage of the penile pump system and right scrotal prosthesis. We noticed a peculiar shape of scrotal part and the neophallus after completed scar maturation and partial shrinking of the flap’s soft tissue (Figure 5A-5C). Before surgery the conservative treatment of the forearm consisted in massages, silicone gel, compression and steroid injection. Preoperative measurements detect a Tinel sign 4cm proximally and 2.5cm distal of the radial innervated field. Nerve conduction revealed a reduced velocity and amplitude of the left affected superficial branch in comparison to the opposite side (left 17.9mV; 59.9m/s vs right 86.3mV; 65.7m/s). Sonographic measurements of the skin layer determined a thickness of 0.9mm over the main branch.
Patient’s expectations on our operative therapy addressed alleviation of the obstructive sensation as well as neuropathic symptoms caused by the rigid circumferential scar area on the donor side, conspicuous aspect of the of the neophallus and left neoscrotum plus ventralisation of the right scrotal prosthesis. After the first operation the Tinel sign was reduced detectable 3.2cm distal and 1.4 proximally from the radial branch and ROM of the wrist improved especially 10° ulnar and radial abduction. The nerve conduction demonstrated a lowering of the amplitude after each fat grafting session, although the velocity persisted low (left 8.3mV; 59.9m/s vs right 85.7mV; 65.9m/s). Thickening of the local skin layer was estimated of 1.3mm by ultrasound. In the second session ACRT-concept on the forearm and penile area was done in combination to ventralisation of the right scrotal prosthesis and lipografting to the neophallus. Stepwise a soften coverage of the penile pump system in the left neoscrotum and widening of the penile circumferential scar have been achieved (Figure 5D-5F). In By loosening the fibrotic entrapment and thickening the subcutaneous layer on the donor side neuropathic symptoms decreased according to a Tinel sign 1.2cm proximally and 1.3cm distal. ROM rapidly improved and reached except 5° in supination painless completion. Questionnaires evaluation estimated a decrease of the Patients baseline POSAS score from preoperatively 88 to 48 as well as VAS scores from 8 (severe pain) to 2 (mild pain). However, he showed no recurrence of erythema, inflammation or wounds in the genital region during the complete follow up. Hence penile diameter increased 0.9cm and stayed stable in shape without problems in urologic or erectile function providing more self-confidence in patient’s sexuality.
Case 3
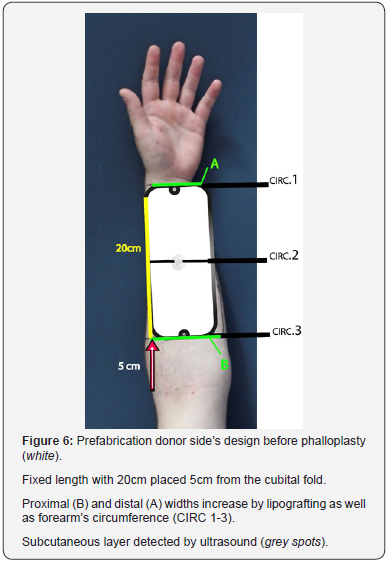
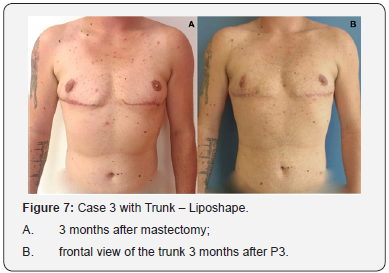
26 years old, smoker (10py) with a BMI of 28.2kg/m2 was planned for mastectomy as the first intervention after one year of hormone therapy. Since FtM patients’ complaints had been reported about postoperative soft tissue shrinking and decreased penile size after radial free flap phalloplasty, we conducted a pre-enhancement before flap harvest through sequential lipografting. The design of the future donor side was marked on the nondominant left medial forearm (Figure 6). We chose larger outlines, i.e. 20cm length in order to correspond an enhanced shape of the “prefabricated” flap after microsurgical transplantation. Preoperative clinical measurements recorded forearm’s circumferences, sonography assessed the thickness of the subcutaneous layer and controlled the vascularity during the prefabrication process on several levels: wrist (CIRC1), half middle forearm (CIRC2) and proximal forearm (CIRC3). In the first procedure the mastectomy and waterjet assisted lipografting of 116cc from the abdomen to the left arm took place. Afterwards hypertrophic scarring and an unpleasant aspect of the right NAC due to partial necrosis and wound healing problems were noticed (Figure 7A). In the second procedure we applied the scar release method to treat the right fibrotic deformed NAC and pectoral scar (23cc) simultaneously with the forearm augmentation through 94cc autologous fat graft harvested from both flanks. In this way we obtained symmetry in the pectoral part and a thickening of the subcutaneous layer of the left forearm. In order to provide a reliable soft tissue enhancement of the future donor side and a masculine aspect of the chest, the patient underwent a third forearm augmentation (96cc) combined to the trunk liposhape approach (Figure 7B). Here we removed 480cc fat from the abdomen, flanks and lateral thoracic area and transplanted 100cc subcutaneously and 70cc intramuscularly to enhance the pectoral muscle contour. Postoperatively forearm’s circumferences showed a mean increase of 2,6cm (ranged 0,8cm to 5,6cm) (Table 2). Furthermore, ultrasound measurements proved intact vascularity by Doppler and a successful engraftment in the “prefabricated” flap area (Figure 8A & 8B). In summary patient maintained excellent functional and aesthetic aspect of the forearm after insertion of 303cc lipograft with the technique described.


T0 = preoperative ; Tx = 3 months postoperative.
Discussion
The most important goal of female-to-male genital reassignment surgery is an inartificial masculine outer aspect accompanied with optimal penile reconstruction, which allows the FtM patients to void standing up and sexually interact with penetration [13,28]. Even though multiple operative steps are taken during the process, remarkable paucity exists concerning specific techniques to address persistent scar related disfigurements, donor side disability with neuropathic pain, trunk contour deformities after mastectomy, dislocation of scrotal implants or tissue expansion in the mean of secondary surgical corrections [29,30]. Our lipografting protocol combined with a minimal invasive scar release called ACRT was performed in the abovementioned three FtM transgender cases to improve the scar related complaints on the donor forearm after free radial forearm flap like rigid adherence, pain sensation in the superficial radial nerve area, decreased ROM, differing pigmentation, shrinking of the subcutaneous fatty layer. Upgraded appearance in scar area as well as a pliant skin texture measured by POSAS scale system, probably lead to complete painless ROM of the donor wrist. Obvious reduction of the neuropathic features registered through VAS Scores, Tinel sign’s exhibition, nerve conduction and ultrasound measurements, seemed to be linked to fat graft’s cushioning (mechanical) and regenerative effect recently described in scars in addition to minimal invasive release of fibrotic tension on the nerve [8,9,31]. Conversely literature reports, that scarring in the forearm’s skin graft do mainly result in functional and pain-free donor side with high patient satisfaction [10,17,18]. We feel, that the ACRTprotocol offers a powerful tool for systematic fibrotic loosening of the scar area without compromising the vascularity of the full skin graft in patients with persistent donor side’s complaints.
Furthermore, this technique was applied to treat aberrant scars due to conservative sex-reassignment mastectomy and radial flap based phalloplasty. In the pectoral area we corrected hypertrophic post-mastectomy scars and regained projection of the nipple. In the genital part we obtained a distension of the inguinal and circumferential penile scars, simultaneous lipografting lead to an enhanced and pendulous shape to the neophallus. Autologous fat transplantation with or without transcutaneous needling of fibrotic tissue has been generally described and proclaimed as promising treatment before [32-34]. Even though systematic transcutaneous needling accompanied by lipografting as synergistic methods in symptomatic scars have not been elucidated in detail or even established as a standard operating procedure(s) (SOP) yet [35,36]. Latter has been established as the ACRT-protocol in our institution for FtM patients with promising results so far. Although controlled randomized studies including a large number cohort are required to verify its evidence.
Scrotoplasty is usually performed with the insertion of silicone implants using the labia majora with or without prior tissue expansion or simultaneous advancement of local skin flaps [37]. Postoperative dislocation of the scrotal implants may provoke skin affections and a hidden aspect of the neoscrotum especially in the lateral view. Poor skin coverage with implant expulsion, mechanical dysfunction or dislocation are known as typical complications after insertion of a hydraulic balanced penile prosthesis [38,39]. To overcome these drawbacks even more surgical interventions and downtime periods are required. In case 2 ventralisation of the right neoscrotum and a cushioning soft tissue coverage over the penile pump system succeeded within short and easy to perform sessions. Follow-ups were uneventful and avert further conservative amendments. The use of lipografing to enhance the subcutaneous skin layer is widely performed in breast surgery e.g. to camouflage the outlines of breast implants [40-42]. However up to date there is no literature reporting the use of autologous fat transplantation for scrotal sequelae in FtM patients.
Ultimately lipografting offered directed soft tissue augmentation for the use of radial free flap prefabrication before phallic construction without notable complications in patient 3. Before different approaches were proposed to derate secondary corrections, functional and aesthetic impairments after phalloplasty e.g. specific closures of the donor side, prelamination with a tube for urethroplasty, or pre-extension by tissue expansion [43-45]. Most techniques include an additional surgical team during time- consuming interventions, notable major complications and prolonged immobilization or demand high patient’s compliance [46,47]. On the other hand, the presented concept of radial free flap prefabrication is surgically feasible as an ambulatory treatment and the forearm’s fatty layer might almost be doubled within three procedures in patients heading to forearm’s flap based phalloplasty. However, the operative approach is presented as a single case so far and must be investigated in a larger cohort including a longer follow up. Finally, pectoral lipografting combined to distinctive liposuction on different parts of the trunk was designed as Trunk Liposhape and led to improved upper masculinization. Our study has limitations such as a low patient number, short follow-up period, observer bias, but this pilot approach provided a first and preliminary impression about reconstructive techniques that have not been described for that patient group so far. Besides, all patients stated that they would undergo the same procedures considering the complications and postoperative results.
Conclusion
Lipografting - if a proper patient selection and operative procedures are applied - is a minimally invasive and patient friendly solution for aesthetic improvement of sequelae resulting from female-to-male sex reassignment surgery. Both symptoms and aesthetic issues create in this specific patient group a large burden in daily and professional life with a permanent reduction of the quality of life or psychological distress. Up to date therapeutic and surgical approaches are limited, that’s why the new concepts had been developed and applied as “rescue” procedures in our department with an acceptable safety profile.
The standard minimal invasive scar release protocol of ACRT combined with or without the Transgender-Trunk Liposhape (TTL) could be used in cases when all previous attempts of conservative treatment have failed. Further clinical studies with large numbered patient groups and recording of a long-term effectiveness are highly recommended and certainly necessary.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment