Juniper Publishers- Open Access Journal of Case Studies
Malignant Arterial Hypertension Revealing Focal Segmental Hyalinosis
Authored by N Mahoungou Mackonia
Abstract
Malignant arterial hypertension (MAH) is a hypertensive emergency associated with grade III or IV retinopathy. Focal segmental hyalinosis (FSH), of late onset, is one of its rare entities, with an incidence of 7 per million, responsible for 15-20% of nephrotic syndromes in adults. We report a case of segmental and focal hyalinosis in a 27-year-old patient with no previous history of malignant hypertension, who consulted us for neurosensory signs and ocular redness. The clinical examination showed a hypertensive peak at 240/150mm Hg with myocardial hypertrophy confirmed by electrocardiogram and transthoracic echo. A fundus examination completed by an optical coherence tomography revealed a KIRKENDAL stage III retinopathy associated with an occlusion of a branch of the central retinal vein. An impure nephrotic syndrome associated with renal failure was observed. A biopsy of a fragment of renal parenchyma supplemented by pathology was performed in favour of FH with chronic tubulointerstitial disease. The patient was managed urgently with nicardipine 3-5mg/hr by electric syringe within 24 hours, followed by a triad of antihypertensive drugs consisting of amlodipine, indapamide and Ramipril at full dose combined with prednisone 60mg/day for 4 months with a 6 month taper. The evolution was marked by a normalisation of the renal function, disappearance of the proteinuria and even a normalisation of his eye fundus after one year. FSH constitutes a group of heterogeneous pathologies with multiple causes, of which malignant hypertension is a secondary one, requiring not only symptomatic but also etiological management.
Keywords: Malignant arterial hypertension; Focal segmental hyalinosis
Abbreviations: MAH: Malignant Arterial Hypertension; FSH or FH: Focal Segmental Hyalinosis; BP: Blood Pressure
Introduction
Malignant arterial hypertension (MAH) is a nosological entity defined by an abrupt rise in blood pressure (BP>180/110mm Hg) associated with grade III or IV retinopathy [1]. It is a hypertensive emergency with a poor prognosis, which has become exceptional nowadays in countries with adequate medical coverage [2]. Malignant hypertension causes multivisceral failure as a result of ischaemia secondary to multiple lesions in the vascular endothelium. Focal segmental glomerulosclerosis, which occurs later than retinal and cerebral damage [1], is one of its consequences. This entity is rare with an incidence of 7 per million, responsible for 15 to 20% of adult nephrotic syndromes [3]. We report a case of segmental and focal hyalinosis in the setting of malignant hypertension.
Case Report
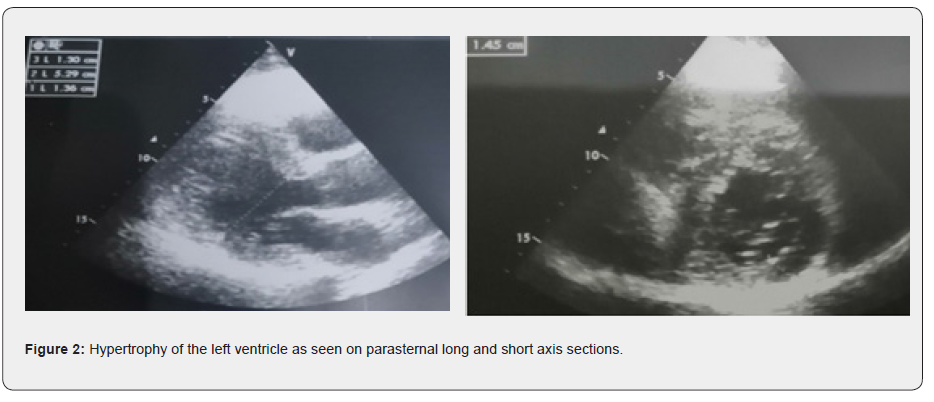
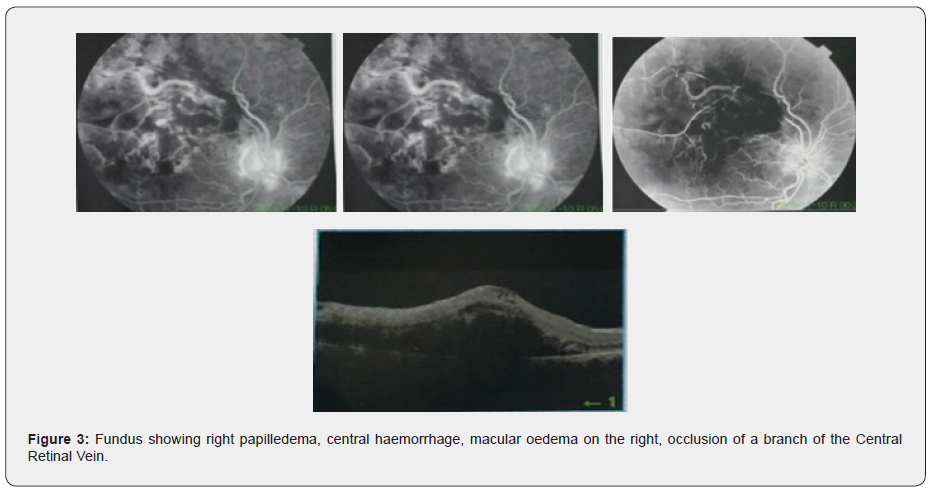
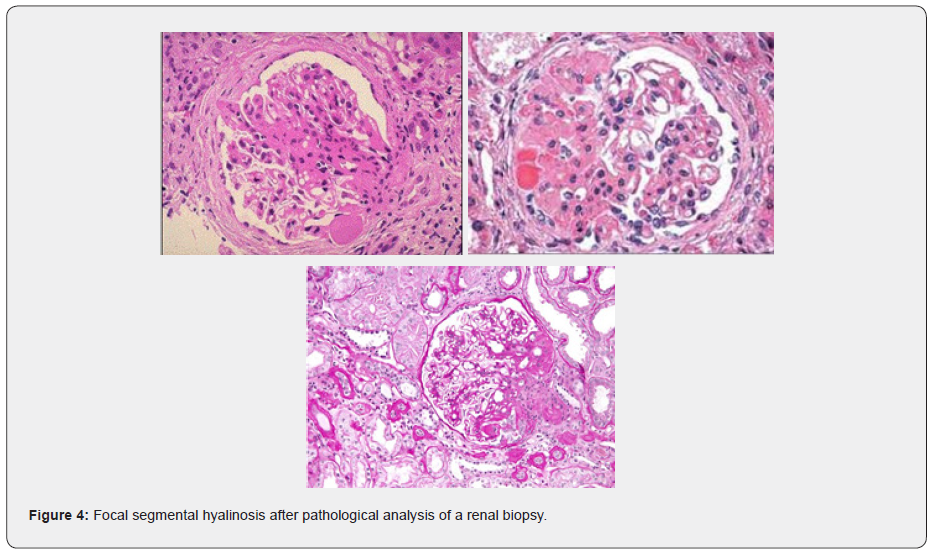
We report the case of a 27 year old patient, with no particular personal or family history and a body mass index of 23kg/m2, hospitalized in the cardiology department for malignant hypertension (hypertension). The diagnosis was made in the presence of headaches, dizziness, palpitations, ocular redness and a sudden drop in visual acuity, which led to a consultation in ophthalmology. The clinical examination revealed a hypertensive peak of 240/150mm Hg with a heart rate of 70 beats/min and discrete oedemas of the lower limbs, whitish in colour, taking the cup. left ventricular hypertrophy was found on electrocardiogram confirmed by transthoracic echocardiography (SIV/VGTD=13mm; PP/VGTD= 13mm). A workup was performed, including a fundus, supplemented by an optical coherence tomography (OCT) scan, showing bilateral papilledema; central hemorrhage predominantly in the left eye; macular edema more to the right and occlusion of a branch of the central vena mater. The biological work-up showed an impure nephrotic syndrome with 24-hour proteinuria at 6.6g/24h, microscopic haematuria (15,000 red blood cells/field) on cytobacteriological examination of the urine, renal failure at 23.5mg/l, GFR at 35.5ml/mn/m2 and urea at 0.81g/l with hypo albuminemia at 27g/l and hypo complement C3 at 0.25g/l and hypertriglyceridaemia at 3g/l. A biopsy of a fragment of the renal parenchyma, completed by a pathological assessment, was carried out in favour of a focal segmental hyalinosis (FSH) with chronic tubulointerstitial damage. The workup for secondary FH was normal, including: methoxylate levels, thyroid hormones, plasma renin, blood aldosterone, blood cortisol, blood glucose, complete serology and complete immunology. Abdominal ultrasound, renal artery Doppler and renal bladder ultrasound were normal as was the abdominopelvic CT scan. The diagnosis of FSH probably secondary to malignant hypertension was made. The patient was admitted to hospital as an emergency, conditioned with monitoring ; Loxen at 3mg/hr to 5mg/hr by electric syringe over 12hrs with an increase of 0.5mg/15min was administered, then relayed by amlodipine 10mg/day, Ramipril 10mg/day and bisoprolol 2.5mg/day. Atorvastatin was administered at 40mg/dr followed by corticosteroid therapy with prednisone 60mg/dr (1mg/Kg/dr) for 4 months with gradual taper for 6 months combined with vitamin D, calcium, potassium supplementation and gastric dressing with pantoprazole 30mg/dr were administered. The patient was admitted to hospital for one week and then discharged with a blood pressure of 130/70mmHg with close monitoring for 1 year. The evolution is marked by an improvement in visual acuity, neurosensory signs and a balance in blood pressure. On the biological level, there was an improvement in renal function (creatinine level at 12mg/l with a GFR of 77ml/mn) with disappearance of the 0.2g/l proteinuria and an improvement in his eye fundus.

Discussion
Focal segmental hyalinosis (FSH) is a rare kidney disease with an incidence of 7 per million. It affects both children and adults with peaks at 6-8 and 20-30 years of age, respectively [3]. FSH is the leading cause of nephrotic syndrome in the United States (accounting for approximately 35% of cases). It is somewhat less common in Europe, 12% in Spain. In 2010, in France, 2.2% of incident patients with end-stage renal disease have FSH (Kidney Registry 2010) [4,5]. FSH is responsible for 15-20% of adult nephrotic syndromes [3]. The onset of nephrotic syndrome in FH is due to a disturbance of renal function because of glomerular damage and scarring. The disease is due not only to glomerular sclerohyaline lesions which may be associated with immunological deposits (IgM, C3) within these lesions, but also to podocyte damage, resulting in the loss of the physical integrity of the filtering barrier. A protein produced by podocytes, called integrin αvβ3, is crucial in 'gluing' podocytes to the structure of the glomeruli.
Dysregulation of the αvβ3 integrin pathway could lead to glomerular filtration dysfunction. Damaged glomeruli allow the passage of large molecules, especially proteins. Nephrotic syndrome is often impure, i.e. associated with hypertension and/or haematuria and/or organic renal failure [3,6,7].
FSH may be primary without any cause found, in which case, AH progressively sets in with the renal disease thus worsening the prognosis, or it may be secondary in relation to several pathologies including viral, drug-induced, genetic, AH, etc.; in this case, AH precedes the clinical picture [4,7]. Thus, malignant hypertension can cause a variety of lesions, including glomerular endothelial and epithelial cell damage, glomerular hyperfiltration, increased renin-angiotensin-aldosterone system, and endothelial-epithelial interaction, leading to the development of secondary FSH and proteinuria, but less so than in the primary forms [7,8]. Only a few clinical studies describe the development of FSH in malignant hypertension and these studies have reported that it can occur in primary malignant hypertension with nephrotic-like proteinuria, and may contribute to renal dysfunction [8]. Early treatment of hypertension is essential with a blood pressure target of 130mmHg systolic and 80mmHg diastolic for patients with significant proteinuria > 1g/24h. High-dose corticosteroid therapy is the first-line treatment of choice in primary FH [9]. But the rare genetic forms are rather cortico-resistant [7].
Our patient was 27 years old, the age favorable for peak FH as reported in the literature. He presented with FH secondary to malignant AH, which can be explained by a very prominent and prominent AH, rarely seen in primary FH. Although no etiology of malignant AH was found in our patient, the evolution was marked by an improvement of the clinical picture under 3 antihypertensive drugs and corticotherapy.
Conclusion
Malignant hypertension is a serious disease with several complications including FSH. The aetiologies are multiple and must be found. The management must be done urgently because it conditions the vital prognosis of the patient.



No comments:
Post a Comment