Juniper Publishers- Open Access Journal of Case Studies
Posterior Thoracolumbar Hemivertebra Resection and Fusion with a Biphasic Calcium Phosphate Bone Graft with a Novel Submicron Surface Topography
Authored by Faheem Sandhu
Abstract
Hemivertebra deformity and tethered cord syndrome are rather rare spinal anomalies and are not frequently reported in adults. The literature reports most cases occurring in children-with hemivertebra occurring in approximately 3-10 of 1000 births as a commonly recognized cause of congenital scoliosis in the thoracic and lumbar spine. Deformity related to the hemivertebra may progress quickly in the early years of life, or it may progress slowly into young adulthood. However, at some point, the negative effects on the spinal cord and the coronal and sagittal balance are likely to require surgical correction involving either anterior–posterior fusion or posterior resection with fusion. Surgeons face many challenges in these surgical cases. One such challenge is having an adequate supply of autograft available for such complex, multi-segment procedures while avoiding additional procedures and increasing operative time. Identifying the most appropriate bone graft is important and the science behind the graft selected should be considered carefully. In recent years, the study of osteoimmunology has demonstrated the effects of the bidirectional interaction between bone cells and the immune system on bone development. In this report, we discuss the case of an adult female patient with a history of tethered cord release and known kyphoscoliosis presenting with a thoracolumbar hemivertebra at T12. The surgical treatment included a posterior resection and posterolateral fusion using this bone graft with a novel submicron surface topography and the radiological fusion findings observed in situ at 6 weeks post-surgery.
Keywords: Hemivertebra deformity, Congenital scoliosis, Osteoimmunology, Immune system, Lumbar spine, Mesenchymal stem cells, Topography
Introduction
Hemivertebra deformity and tethered cord syndrome are rather rare spinal anomalies and are not commonly reported in adults [1,2]. The literature reports most cases occurring in children with hemivertebra occurring in approximately 3-10 of 1000 births as a commonly recognized cause of congenital scoliosis in the thoracic and lumbar spine [3,4]. The deformity is the result of the failure of the vertebra to develop fully, which causes abnormal shaping of one or more affected vertebral bodies, or sometimes a failure of vertebral segmentation. Progression of hemivertebra may be rapid in the early years of life, or it may simply progress slowly into young adulthood. Nevertheless, at some point, the negative effects on the spinal cord and the coronal and sagittal balance often require surgical correction involving either anterior–posterior fusion or posterior resection with fusion. Surgeons face several challenges in these surgical cases, one of which is having an adequate supply of autograft available for such complex, multi-segment procedures. Another challenge for surgeons comes in identifying the most scientifically advanced bone graft alternative for the procedure to avoid added operating time and the known complications inherent in harvesting autograft [5]. The synthetic calcium phosphate bone graft closely resembles human cancellous bone and has an exceptional safety profile and has proven to be a cost-effective alternative to autograft [6-8].
The body’s natural response to tissue injury caused by spinal surgery is the upregulation of pro-inflammatory macrophages (“classically activated M1 macrophages”) which are the first-responders of the immune system. If that inflammatory response becomes chronic there is a risk of fibrosis, non-union and the development of a pseudarthrosis in spine fusion defects. The unique needle-shaped submicron surface of this novel biphasic calcium phosphate (BCP) polarizes naïve monocytes to the pro-healing and anti-inflammatory M2 phenotype of macrophage, which leads to the upregulation of mesenchymal stem cells and the formation of bone rather than scar tissue [9].
In preclinical studies, this BCP has been shown to promote bone formation, even in soft tissue, without the need for added cells or growth factors [9]. This novel BCP bone graft is designed to mimic the porous, trabecular structure of cancellous bone and bone formation takes place throughout the BCP bone graft leading to a uniform, solid, and stable fusion which has been found in clinically-relevant animal studies [10,11].
The report described herein is that of an adult female patient with a thoracolumbar hemivertebra surgically treated with resection and posterolateral fusion using this novel bone graft with submicron surface topography and the radiological fusion findings observed in situ at 6 weeks post-surgery.

Case Description
The patient is a 54-year-old female nurse with a history of tethered cord release and known kyphoscoliosis with T12 hemivertebra who presented with progressive urinary incontinence and lower extremity weakness/numbness over the past year. The surgery included a planned resection of a segmented T12 hemivertebra with shortening of the spine and T8-L3 fusion.
Surgical Procedure
A standard posterior resection of the hemivertebra was performed at T12 along with curve correction at T8-L3. Following a midline incision, the hemivertebra and posterior spinal elements to be fused were identified. Pedicle screws were placed from T8 to L3, omitting the T12 and the right L1 screws due to atretic pedicles. Removal of the hemivertebra and decompression were carried out carefully at T12. Pre-contoured rods were secured to the screws. Decortication of the posterior elements was completed, and MagnetOs bone graft was placed over the decorticated bone along the lateral gutters from T8-L3. BCP granules were mixed with morselized local autograft from the excised hemivertebra and spinous processes. The entire procedure was performed under neuro-monitoring to continuously assess and prevent damage to neural structures.
Postoperative Course
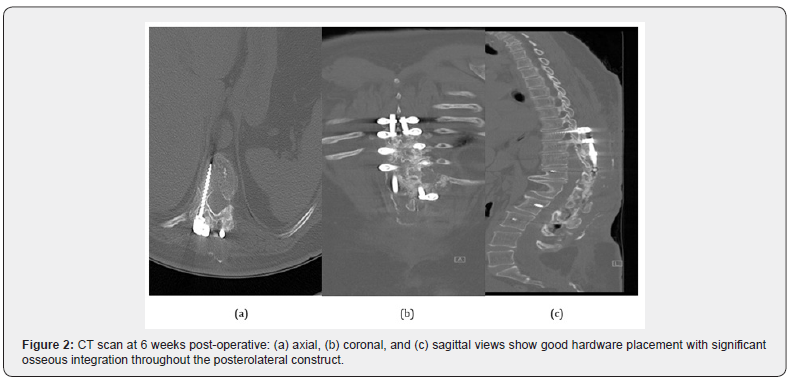
The patient had an initial uncomplicated postoperative course but developed increased pain and swelling around her incision at four weeks that increased over the next two weeks. She was seen at this time in the clinic with complaints of incisional pain and lower extremity paresthesias. Her wound was intact, but tender to palpation and there was fluctuance in the soft tissue. A CT scan was taken to evaluate for a possible seroma. The CT scan confirmed the presence of a seroma while also demonstrating a considerable fusion mass. The patient was taken back to the OR for the evacuation of the seroma. During the evacuation procedure, exploration of the fusion mass was carried out at the same time, which revealed the BCP granules to already be quite solidly fused.
Discussion
A wedge-shaped hemivertebra is known to lead to a higher risk of the progression of scoliosis deformity as was presented in this patient along with associated neurologic findings. Resection with instrumented posterolateral fusion corrects the curvature and provides stability to the involved vertebral segments. A harvest of local, or iliac crest bone graft in sufficient volume for a multi-level fusion procedure is often prohibitive due to the volume of autograft bone required for each of the levels to be fused, as was the case for the patient described herein. Although synthetic bone graft options have historically performed less well compared to autograft [12], this case exhibits the benefits associated with the use of this biphasic calcium phosphate with needle-shaped submicron surface topography in achieving a reliable and solid fusion.
The outcome reported in this case of a middle-aged female patient that progressed to successful fusion early in the postoperative course, not only radiologically, but also upon manual confirmation during the subsequent surgical procedure, further demonstrates that this BCP bone graft with needle-shaped submicron surface topography is an effective bone graft extender for use in posterolateral spine fusion [13].
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment