Juniper Publishers- Open Access Journal of Case Studies
Reversible Posterior Encephalopathy Syndrome Remission with the Complete Response in a Patient with Multiple Myeloma after Continuous Application of Bortezomib
Authored by Li Bao
Abstract
Introduction: Bortezomib is the first generation of proteasome inhibitors and is a cornerstone drug approved for the treatment of multiple myeloma, recommended by the NCCN front-line (IA).
Case Presentation: A 61-year-old man was first attended to our hospital due to “low back and rib pain for 3 months”. He had renal insufficiency (creatinine 357μmol/L, urea nitrogen 18.8 mmol/L). After bortezomib therapy, he had altered mental status, seizures and aphasia. He was diagnosed with multiple myeloma IgG- λ light chain stage III B (DS staging) III (ISS staging), acute renal injury; posterior reversible encephalopathy syndrome. Electrocardiogram monitoring, oxygen inhalation, mannitol for dehydration were administrated. Sodium bicarbonate tablets (1mg bid), and the hydration treatment were still given to the patient, and he was suggested to drink proper water considering his poor heart and renal function.
Discussion: Proteasome inhibitors have previously been reported to cause reversible posterior encephalopathy syndrome, but the mechanism is not clear. However, we consider that the complication in this patient is caused by many factors, proteasome may not be the cause of the disease. After persistent application, the disease has been alleviated, and the reversible posterior encephalopathy syndrome has been improved. Furthermore, he exhibited very good response (VGPR) under continued bortezomib (iv once a week) therapy based on our follow-up.
Established FactsProteasome inhibitors have previously been reported to cause reversible posterior encephalopathy syndrome, these cases all stopped application of bortezomib, and their conditions deteriorated as evidenced by a period of follow up.
Novel InsightsNot all cases of PRES were caused by bortezomib. This is the first report of a patient that does not withdraw or replace bortezomib when facing PRES, and owing to bortezomib, his MM condition got clinical remission, and was accompanied by concomitant improvement in the renal function miraculously
Keywords:Bortezomib; PRES; Remission; Multiple myeloma
Introduction
Bortezomib is a cornerstone drug approved for the treatment of multiple myeloma (MM), recommended by the NCCN front-line (IA) and widely used at home and abroad [1,2]. The most common adverse reaction is peripheral neuropathy, which attracts great attention in clinical practice [3]. However, there are few reports of central nervous system lesions, posterior reversible encephalopathy syndrome (PRES) is one of them. The clinical manifestations of PRES comprise unexplained headache, blurred or low level of consciousness, visual changes, epileptic seizures, intractable hypertension, and characteristic neuroimaging manifestations of posterior white matter edema [4].
We herein report on a PRES case occurred in the bortezomib therapy of multiple myeloma. Clinicians should weigh and consider the balance of risks and benefits, as we look forward to a wider and safer application of bortezomib in hematological disease.
Case Presentation
In August 2018, a 61-year-old man was first attended to our hospital due to “low back and rib pain for 3 months”. He had hypertension for 20 years, peak blood pressure could reach 180/110mmHg, and has taken metoprolol tartrate tablets 25mg twice a day for a long-term administration, his blood pressure was controlled at 150/70mmHg for a long time. He had diabetes mellitus for 5 years, and now takes metformin 1000mg 6AM, but was not well controlled. He has mitral valve prolapse with regurgitation for 5 years but wasn’t given special treatment. Atrial fibrillation for more than 3 years, with no anticoagulant drug. Physical examination after admission showed clear mind. The tremors could be touched in the precordial area. Abdomen is soft, but tenderness and rebound pain exist in the left lower abdomen. Laboratory evaluation suggested that the patient had hypercalcemia (calcium 3.64mmol/L), renal insufficiency (creatinine 357μmol / L, urea nitrogen 18.8mmol / L), hyperuricemia (uric acid 814μmol / L), hyperglycemia (glucose 12.0mmol/L), moderate anemia and thrombocytopenia. Serum IgG 41.40g/L, IgA 0.15g/L, IgM 0.11g/L, complement C30.78g / L, κ light chain 1.36g/L, λ light chain 24.90g/L, urine κ and λ light chain were undetectable, blood immunofixation electrophoresis (IFE) showed IgG-λ monoclonal band and a light chain λ monoclonal band. Urinary IFE showed a monoclonal band of free light chain λ. Bone marrow biopsy showed CD38+ plasma cells 34.8%, expressing CD45dim, CD38, clambdaCD138, PCR showed MAGE-C1/CT7(+), bone marrow showed immature plasma cells 93%. Echocardiography showed LVEF was 66%. FISH result (CCND1, 1q21, p53, 13q-, FGFR3, MAF) was normal.
The patient was diagnosed as multiple myeloma IgG- λ light chain stage III B (DS staging) III (ISS staging); acute renal dysfunction; hypertension grade 3 (very high risk); type 2 diabetes mellitus; atrial fibrillation and hypercalcemia. In light of the diagnosis and echocardiographic results, we decided to treat this patient with PAD plan, that is bortezomib (1.3mg/m2, 2.5mg weekly i.v.) in combination with dexamethasone (40mg, d1-4, i.v.) and liposome doxorubicin (40mg, d1, i.v.), which started on August 7th, 2018. At the same time, Sodium bicarbonate tablets (1mg bid), low-molecular-weight heparin and the hydration treatment were given to the patient, and he was suggested to drink proper water during the day.
On August 12th, five days after the first infusion of bortezomib, he acutely developed altered mental status, drowsiness, accompanied by intermittent restlessness and expression indifferent. A neurological examination showed aphasia, adjustment and convergence reflexes disappearing. Laboratory test revealed hypercoagulable state of blood (fibrinogen 133.6mg/ dl, D-Dimer 0.55mg/l FEU). Cerebral computed tomography (CT) scan was failed to perform due to his restlessness. On August 13th, the vital signs were stable, but the mental status did not improve significantly, accompanied by occasionally cough. Physical examination showed sleepiness, delirium and failing to communicate. No seizures had been observed and his blood pressure fluctuation was between 140-152/80-96mmHg. There was no obvious abnormality in the blood ammonia, electrolytes level and imaging examination. Nuchal rigidity was present, and 3 fingers were engraved onto the chest. Cranial CT showed multiple bone destruction of skull with small nodules at the top of the skull, considering MM metastasis, and senile brain changes. Craniocerebral magnetic resonance imaging (MRI) plain scan plus diffusion showed senile brain changes and multiple bone destruction of skull. The imaging examination above demonstrated no new lesions compared with before in the year of 2018. In view of the urgent need for the treatment of multiple myeloma, after fully communicating with family members, the second dose of bortezomib was still given on August 14th. Dramatically, over two preceding days, his state of mind and spirit improved day by day, and the vital signs were stable until 16th. Physical examination showed mental clarity, but he was found to have a right deviation of the tongue. Previous data exhibited that there were reports of disturbance of consciousness caused by drug-induced white matter lesions, so chemotherapy was suspended, and then the changes of the patient’s condition were closely observed. On the 19th, cranial MRA showed no obvious abnormality. Whereas a repeat examination of the cranial MRI suggested mild white matter degeneration. During this period, the symptoms had improved a lot except for the deviating tongue, and patient’s family agreed to continue the chemotherapy, so we gave the third dose of bortezomib in this course of treatment. The creatinine of the patients was significantly lower than that before admission. He achieved clinical remission after 3 cycles of regimen and had clear speech, however, his right tongue did not recover.
Discussion
PRES is a rare but fatal clinic-radiological syndrome associated with reversible nervous system impairment and typical imaging alterations, was first put forward by Hinchey in 1996 [5]. However, its pathophysiological mechanism is the subject of ongoing investigation. Causes include accelerated hypertension (most common); all kinds of serious kidney diseases (acute glomerulonephritis, chronic renal failure); employment of immunosuppressive agents or cytotoxic drugs, such as immunoglobulin, interferon, cyclosporine, after organ transplantation; and so on [6]. It can be visible at any age, more often in young females. Clinical features contain a sudden elevation of blood pressure; headache; visual disturbance; seizures and altered mental status [7]. CT scan lacks specificity, MRI shows angiogenetic edema in both posterior cerebral hemispheres [8]. Diagnosis depends on predisposing factor, reversible symptoms and radiography. Delay of recognition diagnosis and treatment would result in permanent sequelae, so prompt diagnosis and treatment are of great clinical importance.
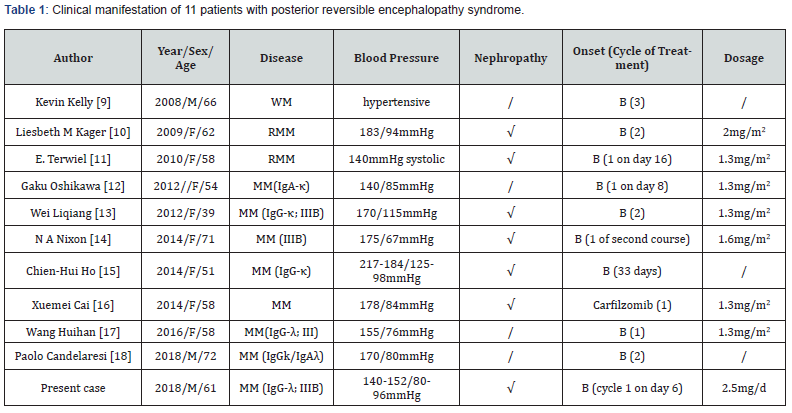
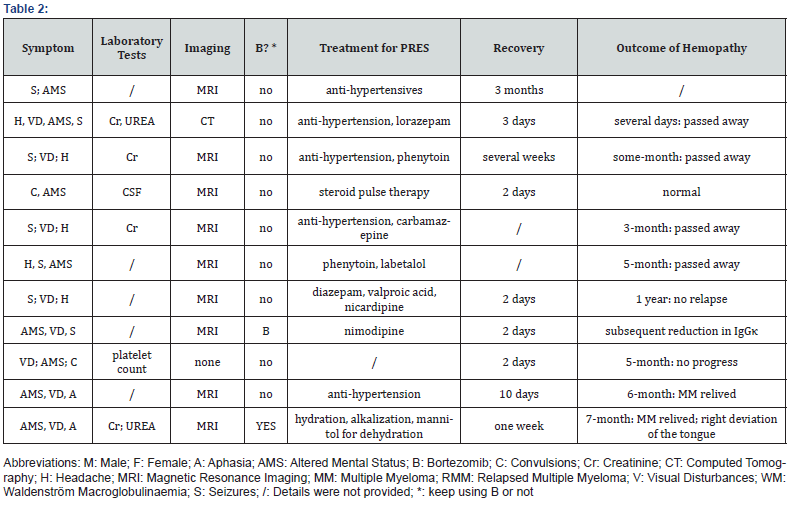
Bortezomib is the first generation of proteasome inhibitors with antiangiogenic and proapoptotic properties, while carfilzomib, newly appears on the market, is the second, they both have been reported to associated with PRES, of which plasma hematological diseases account for eleven cases, one was Waldenström macroglobulinaemia, a kind of inert small granulocyte lymphoma, the other ten were all MM (including this case).
The characteristics of total eleven cases related to bortezomib reported are outlined in Table 1 & 2 [9-18]. Among these cases, male only account for 3/11; all experienced hypertension during PRES attacks; a half mentioned had varied degrees of renal injury; all of them had specific clinical features and imaging changes. Their treatment for PRES was essentially symptomatic, such as anti-hypertension and sedatives. Improvement or complete resolution of changes on repeat neuroimaging and clinical status are relatively constant findings.
We herein present a newly diagnosed and treated MM patient who had headache, visual disturbance and an altered mental status five days after the first dose of bortezomib use. CT and MRI excluded the possibility of intracranial space occupying lesion, cerebral hemorrhage and infarction. A presumptive diagnosis of PRES was made due to the typical symptoms and mild white matter lesions of MRI. Optical microscope morphological observation and Hoechst33258 nuclear fluorescence staining results showed bortezomib of 0.03μM, 0.3μM and 3μM could dose-dependently induce apoptosis in primary cultured cerebral cortical neurons of rats [19], suggesting that bortezomib could go through the blood brain barrier and accumulate in the brain, damaging the nervous system. Considering the high correlation in time and the nervous system damage of bortezomib, bortezomib has become a key suspect in causing this comorbidity.
We thought in-depth what was the real causes of this patient’s PRES? Most of PRES occur when the overall conditions of patients are poor. In the same time, it needs to be taken into account that first, this patient had MM, free light chain, uric acid and calcium might deposited in kidney, leading to a high level of creatinine, but we didn’t pay close attention to hydration at the same time of chemotherapy, resulting in progressive deterioration of renal function. Second, this patient had a long term of hypertension, his blood pressure fluctuated at around 150/90mmHg during hospitalization. They are all stablished causes of PRES. Although PRES occurred after the use of bortezomib, the drug seemed to act as the last straw of the occurrence of PRES. We assume that the past diseases mentioned above together with the additional effects of bortezomib synthetically contributed to the occurrence of PRES.
Generally speaking, the clinical process of PRES is reversible and the prognosis is good. The overall prognosis depends on the condition of underlying diseases [20,21]. Through literature review, we found that there were 4 cases that didn’t have further treatment for MM during the recovery of PRES, their conditions deteriorated as evidenced by a period of follow up, unfortunately, they ultimately passed away from progressive myeloma. Based on these considerations, we intended to continue to use bortezomib to treat MM in this case, after communicating with his family the risks and benefits of bortezomib, his family agreed to continue the drug. When we continue to use bortezomib, his nervous symptom became remission, so bortezomib might not be the arch-criminal of PRES.
In contrast to the other ten cases, this case is unique in continuation treatment of bortezomib after recovery of clinical symptoms. This is the first report of a patient that does not withdraw or replace bortezomib when facing PRES. Since then, the symptom resolved except for right deviation of the tongue and MRI performed 7 months later still had white matter lesion in bilateral lateral ventricle. The cause of not completely recover might be contributed to the continuation of bortezomib or other factors mentioned above, it is a comprehensive outcome that couldn’t blame on the use of bortezomib. But these irreversible symptoms don’t influence patient’s daily life, and owing to bortezomib, his MM condition got clinical remission, and was accompanied by concomitant improvement in the renal function miraculously. For patients who are first diagnosed with PRES, especially accompanied by renal failure, doctors should keep a careful eye on the lipid intake and output and give prompt administration of hydration to prevent excessive blood drug concentration. Continuous administration under effective control is advised because bortezomib is a very efficient drug for MM.
Conclusion
Programs comprising bortezomib are increasingly being used in treatment for plasma cell disorders, so physicians, as well as pharmacists, should be alert to the complication caused by bortezomib and be aware of the relationship between PRES and bortezomib. PRES is caused by comprehensive factors, doctors need to screen carefully whether PRES is associated with bortezomib or not. Bortezomib should not be rudely rejected, so that patients cannot get relief from the disease.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment