Juniper Publishers-Open Access Journal of Case Studies
Mature Cystic Teratoma in the Mediastinum
Authored by Safiyah Noor Zubair
Abstract
This case is a presentation of mature cystic teratoma (MCT) in the mediastinum. A 24-year-old female presented with acute, sharp, and non-radiating chest pain, and anxiety. Her lab findings were significant for elevated WBC, ESR, and CRP. X-ray and CT scans of chest revealed a fat-containing mass in the anterior mediastinum extending to the lung and compressing the pulmonary artery. The mass was subsequently resected via thoracic surgery. Further pathology study revealed skin folds establishing the diagnosis of MCT. This case emphasizes the need for clinicians to include mature cystic teratomas in the differential diagnosis.
Keywords: Teratoma; Mediastinum; Median sternotomy; Mature; Cystic
Abbreviation: MCT: Mature Cystic Teratoma
Introduction
Teratomas are germ cell tumors encompassing multiple cell types from one or more germ layers and can range from well-differentiated (mature) cystic lesions to solid and malignant (immature) lesions [1-3]. They may contain skin with hair follicles and sweat glands, pockets of sebum, blood, fat, bone, nails, teeth, eyes, cartilage, and thyroid tissue [4].
Case Presentation
A 24-year-old female presented to the ER with chest pain, anxiety, and dyspnea starting the day prior. The chest pain was constant, sharp, and non-radiating, with no fever, chills, weight loss, or night sweats. The patient was otherwise in good health. Her past medical history includes epilepsy and a cholecystectomy. Her mother had history of breast cancer. Her vital signs included a pulse of 104, BP 104/70, temperature 36.8°C, resp 16, O2 sat 99%, and BMI of 34.2. She appeared alert, well-nourished, and in no apparent distress. Her lung exam showed decreased breath sounds in the left lung. The rest of the physical exam was benign. Her WBC was 20.7, with no eosinophilia; ESR was 45 and CRP was 11.10. D-dimer was elevated. CEA, AFP, and Beta HCG were negative. Remaining labs were unremarkable; Cocci serology and the HIV and rapid COVID-19 tests were negative.
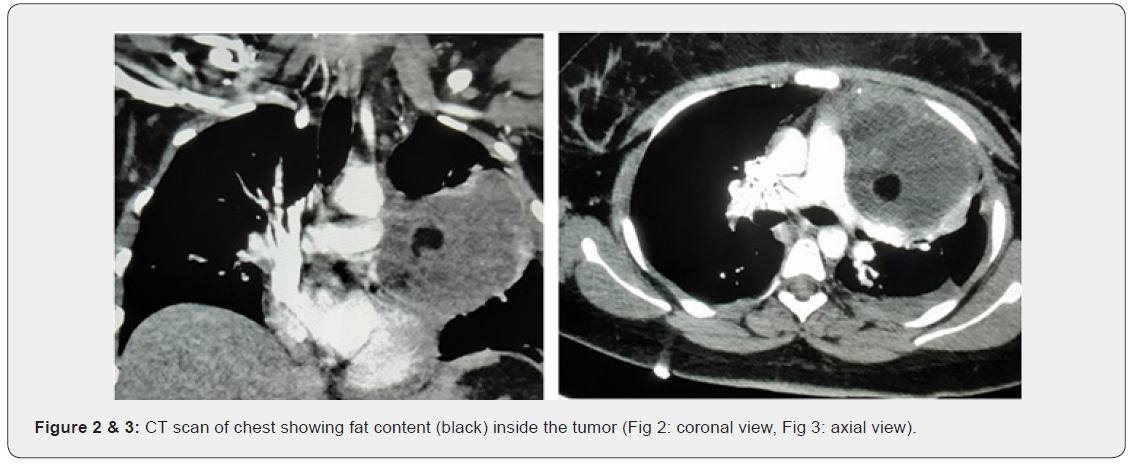
A chest X-ray revealed a left basilar and left mid-lung opacity (Figure 1). CT Angiogram of chest confirmed a complex fat-containing 8cm collection present in the left anterior upper chest extending into the anterior mediastinum and compressing the left pulmonary artery, with a small left free pleural effusion and no consolidation of pneumonia (Figure 2 & 3). CT abdomen and pelvis did not reveal any other suspicious mass or adenopathy. CT head was unremarkable. Differential diagnoses included abscess, hydatid cyst, mediastinal adenopathy with necrosis, germ cell tumor, congenital cyst, necrotic lymphoma, other primary or metastatic malignancy, pulmonary coccidiomycosis, and tuberculosis.
The patient was then seen by pulmonology, infectious disease, and cardiothoracic surgery. CT-guided lung biopsy and aspiration revealed a 4-cc brownish fluid aspirate. Flow cytometry revealed a hypocellular sample with some erythrocytes, neutrophils, and rare lymphocytes; no monoclonal B-lymphocytes were detected. Pathology revealed fibrosed cyst wall histiocytes, negative for malignancy; AFB acid-fast and GMS fungus stains were also negative. Her echinococcus antibody was positive, but no apparent signs of parasitic infection were noted, including no history of international travel. Later, the patient was transferred to a higher care facility where thoracic surgery was performed with a median sternotomy surgical approach.
During surgery, an aspiration of 100-cc of greenish pus was obtained. The contents of the mediastinum anterior to the pericardium were dissected with the mass, including the left half of the thymus. The mass was compressing the left pulmonary artery and was intimately associated with both the main pulmonary artery and the phrenic nerve. The mediastinal mass was excised with left upper lobe wedge resection. Lung fluid Gram stain showed many WBCs and no organisms. Final culture showed no growth. Examination of one fragmented portion of tissue revealed multiple circular portions of skin with a yellow glistening cut surface. Sectioning of the tan-red disrupted tissue revealed white fibrous to hemorrhagic cut surface. A diagnosis of MCT was made.

During hospitalization, the patient was started on ceftriaxone and fluconazole, which were later discontinued. She was discharged on empiric albendazole until the histopathology results returned.
Discussion
A 24-year-old female presented with acute and sharp chest pain, and an anterior mediastinal mass was found and diagnosed as an MCT. Her labs were unremarkable except for a high WBC, ESR, CRP, and D-dimer. CT Angiogram of chest revealed presence of fat in the cyst. The patient underwent open thoracic surgery for excision of the mediastinal mass and wedge resection of the upper lobe of the left lung, and further pathology testing identified skin folds in the cyst.
Several MCTs involving the lung have previously been reported [5]. MCTs, also known as dermoid cysts, are often found in the ovaries and testes, and are rarely found in extragonadal locations such as the chest; less than a hundred cases of teratomas in the lung have been reported [5]. MCTs can occur outside of the gonads when fetal development germ cells fail to migrate down the midline path along the urogenital ridge as ovarian or testicular cells [1].
This case demonstrates that cystic teratomas can involve mediastinal structures; there is compression of the left pulmonary artery and intimate association with the main pulmonary artery and the phrenic nerve. Our MCT consists primarily of skin, an ectodermal component. CTs have high sensitivity in diagnosing cystic teratomas [4]; in our case, it revealed fat but no other components such as teeth or bone. Treatment is largely surgical.
This case emphasizes the need for clinicians to include cystic teratomas in the differential diagnosis. Furthermore, malignant transformation can occur in 1-3% of MCTs [2]. Many of these malignant transformations result in squamous cell carcinomas [2].
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment