Juniper Publishers- Open Access Journal of Case Studies
Odynophagia after Upper Endoscopy: Uvular Necrosis
Authored by Runa D Watkins
Case Report
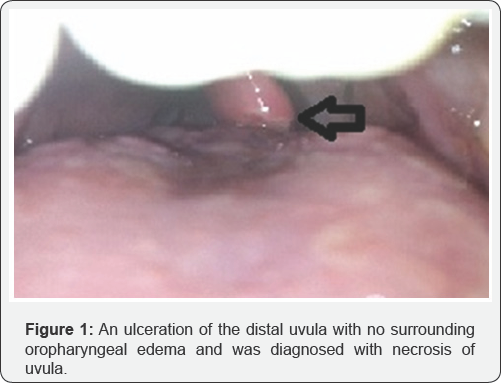
An 8 year old female with DM1 and Celiac Disease underwent an esophagogastroduodenoscopy (EGD) to follow up for mucosal healing on a gluten free diet and presented with throat pain after the procedure. No complications were noted during the procedure, with exception of increased secretions, requiring suctioning at bedside after completion of the procedure. She noted odynophagia the next day with no fever, vomiting or abdominal pain. There was no dyspnea or other respiratory concerns, but parents did note a change in her voice after the endoscopy. She was treated with Acetaminophen, topical throat sprays and swish/spit mixture of Diphenhydramine and Maalox without improvement. Evaluation by ENT showed an ulceration of the distal uvula with no surrounding oropharyngeal edema and was diagnosed with necrosis of uvula (Figure 1). She was treated with topical Lidocaine and Tylenol. She had gradual improvement over the following week after the dependent portion of the uvula was sloughed off.
Uvular necrosis is a rare complication that can occur after an EGD, direct laryngoscopy or aggressive oral suctioning. The mechanism of injury is thought to be due to ischemia, from impingement of the uvula by the instrument against the hard palate or posterior pharynx [1]. Sore throat after tracheal intubation is a common event with an incidence between 24 and 100%. A recent prospective evaluation of 809 patients found it to occur in 40% with an average duration of 16 ± 11 hours postoperative. However, a very severe or persistent sore throat is much rarer and in these cases, uvula necrosis should be part of the differential diagnosis especially with worsening oropharyngeal pain and foreign body sensation [2-4].
Ulcerations can lead to airway compromise, bleeding or sepsis, but resolution of symptoms occurs within 5-14 days. We recommend conservative management with analgesia. The uvula regains its normal appearance and these patients have good clinical outcomes [5]. Rarely, severe cases require parenteral antibiotics and steroids.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment