Juniper Publishers- Open Access Journal of Case Studies
Understanding Optical Coherence Tomography (OCT) is Crucial in the Diagnosis of Adult-Onset Foveomacular Vitelliform Dystrophy (AOFVD)!
Authored by Mina Abdelmseih
Abstract
A case of adult-onset foveomacular vitelliform dystrophy is described in a 65-year-old male patient presented with a gradual unilateral central scotoma in his left eye without any precipitating factors. His vision was 20/30 in the left eye (OS). An optical coherence tomography (OCT) scan revealed accumulation of vitelliform lesion in a cystic space at the retinal pigment epithelium. This case is unique because my patient was previously misdiagnosed as neovascular age related macular degeneration and prepared for further management with intravitreal injections. Successful OCT image interpretation was the major milestone in the accurate diagnosis and management of (AOFVD).
Case Report
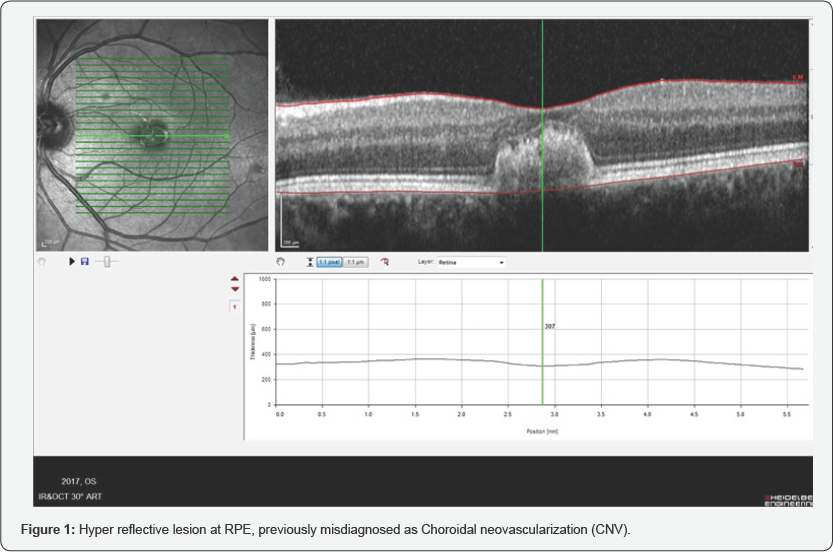
A 65-year-old Caucasian male presented with slowly progressive Painless loss of vision in his left eye over several decades without any precipitating factors. He was referred to me for further management with anti-VEGF therapy for the treatment of neovascular age-related macular degeneration OS (Figure 1, as shown below). Blood pressure (BP) was normal, and there was no history of any systemic diseases as hypertension, diabetes, medications, allergies, Straining or any family history of eye diseases.
The best corrected visual acuity (BCVA) for far and near was 20/20 OD and 20/30 OS. Pupillary responses were equal, round and reactive to light with no afferent defect O.U. Extraocular muscle movements were normal and unrestricted in all positions of gaze O.U. Cover test demonstrated orthophoria at distance. Amsler grid was unremarkable in the right eye, but revealed central metamorphopsia in the left eye.
Gross inspection of the face and lids was negative for ecchymosis, edema or asymmetry. Anterior segment evaluation on biomicroscopy revealed that the eyelids and lashes were clear without evidence of inflammation. The corneas were clear and without evidence of scarring, edema, neovascularization, infiltrates or dendrites. The bulbar and palpebral conjunctivae were clear without injection, chemosis, melanosis, papillae or follicles. The anterior chambers were deep and quiet with absence of cells or flare, hyphema or hypopyon. The irides were flat and without transillumination defects or other signs of atrophy, tears, nodules or neovascularization. No posterior synechiae were present. Anterior chamber angles were estimated to be grade 4 O.U. by the Van Herrick method. Intraocular pressure measured 14/15mmHg O.U. at 4:47p.m.
A dilated posterior segment evaluation of each eye revealed mild cortical senile cataract. No red or white cells were found in the vitreous of either eye and there was no evidence of posterior vitreous detachment or syneresis. Dilated ophthalmoscopy with did not reveal any retinal holes, tears, detachments or vitreous traction. The optic nerve measured 0.4mm in the horizontal and vertical meridians, and was pink, well-perfused and round with distinct margins in both eyes. I saw no notching, bean podding, Drance hemorrhage or retinal nerve fiber layer loss in either eye.
The macula of the right eye was unremarkable and demonstrated a positive foveal reflex. However, a macular exam of the left eye revealed a disinterestedly yellow-orange, vitelliform elevated subretinallesion. An optical coherence tomography (OCT) scan showed that a vitelliform hyperreflective lesion accumulated in a cystic space at the level of RPE (Figure 2, as shown below).
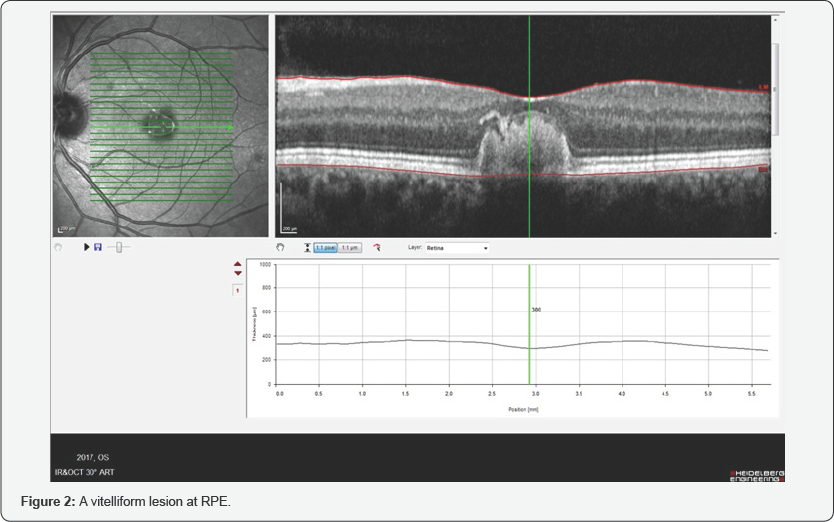
OCT is performed to confirm my diagnosis as AOFVD and to exclude neovascular age-related macular degeneration (NAMD) therefore immediate consultation and appropriate discussion about new diagnosis was done to explain the natural history of disease and eliminate the need for unnecessary invasive procedures as repeated intravitreal injections.
Management
Unfortunately, there is no medical or surgical management for AOFVD. Low vision aids are often needed. Anti-VEGF therapy for CNV has shown potential for improving outcomes, and photodynamic therapy has been used as well. Gene therapy is currently being researched as a possible treatment.
Differential Diagnoses
Neovascular AMD
Neovascular AMD is an acute onset and rapidly progressing disease which affects central vision. Early detection of disease onset and continuous follow-up are mandatory. OCT supports the diagnosis of exudative AMD at initial presentation. The neovascular membrane is localized behind the RPE, creating a vascularized fibrovascular or serous PED [1]. Classic CNV on OCT can present as highly reflective fibrovascular tissue with irregular yet defined borders between the RPE and Bruch's membrane, or above the RPE Likewise, CNV may also present as a localized fusiform serous or fibrovascular PED. CNV not well defined by fluorescein angiography, or occult CNV, may present as RPE elevation from the underlying choroidal plane and may be composed of either serous or fibrovascular tissue [2].
Best vitelliform macular dystrophy
Best vitelliform macular dystrophy is a slowly progressive macular dystrophy .it starts usually in childhood and sometimes in later teenage years. Initially, they have normal central vision followed by decreased visual acuity and metamorphopsia. The diagnosis of Best vitelliform macular dystrophy depends on fundus appearance, electro-oculogram (EOG), and family history Affected individuals have a typical yellow yolk-like macular lesion on fundus examination [3]. OCT imaging has shown that the characteristic vitelliform lesions of BVMD are the result of the accumulation of material in the subretinal space above the RPE and below the outer segments of the photoreceptors [4].
Central serous chorioretinopathy with subretinal fibrin
Central serous chorioretinopathy (CSCR) described as neurosensory detachment of the macula. Fibrin accumulation 10.19080/JOJCS.2018.06.555688 in the subretinal space is an unusual and heretofore unreported visually damaging manifestation of severe CSCR. Optical coherence tomography (OCT) showed a serous elevation of the retina and a shallow RPE detachment, with subretinal accumulation of highly reflective material (presumably fibrin)[5]
Fundus flavimaculatus (FFM)
Fundus flavimaculatus (FFM) is characterised by late onset and slow progression. Yellowish-white deposits called retinal "flecks" are usual features of FFM. These flecks are small or large, extremely polymorphous, rounded, fusiform, spear-like, pisciforms, giants, butterfly or X shaped, and can be juxtamacular or diffusely distributed in the fundus. On Stratus OCT, the retinal flecks presented as small hyper-reflective lesions located either at the inner part of the RPE layer (type 1) or at the level of the ONL (type 2) [6].
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment