Juniper Publishers- Open Access Journal of Case Studies
Significance of STEADI Fall Screening in Early Identification of Geriatric Patients with Undiagnosed Depression
Authored by Anu Garg
Abstract
Background: Clinically overt depression is relatively uncommon among older adults, but it has been identified as a major risk factor for falls.
Objective: The purpose of this quality improvement project is to study and reduce the risk of falls. STEADI (Stopping elderly accidents, deaths and injuries) fall screen and the PHQ-9 (Patient health questionnaire) depression screening questionnaire are used for early identification of patients with undiagnosed depression.
Methods: Using Plan-Do-Study-Act (PDSA) quality improvement methodology, a retrospective chart review was completed from June 2017 until Nov 2018. STEADI fall screens and PHQ-9 depression screening questionnaires of the Community-Dwelling elderly Population seen at the Geriatric Outpatient Clinic at the University of Toledo Medical Center (UTMC), were reviewed.
Results: A total of 4,585 charts of patients (1890 (41.1%) Males and 2695(58%) Females) over 65 years of age seen at the Geriatric Outpatient Clinic at the UTMC were reviewed. On reviewing STEADI fall screens of the total study population, 2709(59%) patients scored (0-3), 828(18%) scored (4-6) while 1048 (23%) scored >7 (High Fall Risk). Depression screening with PHQ-9 was done in 3182(69%) patients while 1403(30.5%) patients were not screened for depression. There were 459 (10%) patients with a negative depression screen PHQ=0 but with a STEADI score >7.
Conclusion: Our study helped us identify opportunities for improvement in our practice. We found that the STEADI fall screen questionnaire can give us information about the functional status of our patients beyond just the fall risk, including identifying patients with underlying undiagnosed depression.
Keywords: Depression; Geriatrics; STEADI falls screening
Abbreviations: STEADI: Stopping Elderly Accidents, Deaths and Injuries; PDSA: Plan-Do-Study-Act; UTMC: University of Toledo Medical Center; PHQ-9: Patient Health Questionnaire; IDT: Interdisciplinary Team
Introduction
Depression is highly common but underdiagnosed among the elderly population, especially those older than 60 years of age. It is associated with other clinical conditions, including cognitive dysfunction and the risk of suicide in the older population [1]. According to the World Health Organization, depression will be the second-leading cause of disease by 2020 [2]. Due to physical and mental decline and frailty secondary to restricted physical activity, the perceived low sense of control over one’s own life renders older individuals more prone to depression [3]. Major depression is considered one of the largest contributors to the global burden of disease. The prevalence of major depressive disorder in the US increased from 13.8 to 25.4 million in the adult population between 2005 and 2010.
This burden has a significant economic impact, costing nearly $77.5 billion in 2005 and increasing to $98.9 billion in 2010, and it is expected to increase [4]. Compared to the younger population, major depression in the geriatric population is more common, presents differently, it is harder to treat, is chronic, and is mostly caused by psychological factors [5]. According to an epidemiological report, the prevalence of depressive disorder and major depressive disorder among patients with cognitive disorders was 11-51% and 15-20%, respectively [6]. For these reasons, it is crucial to identify depression and treat it during the earlier course of the disease to prevent devastating complications in the geriatric population.
Falls and depression are common geriatric syndromes that are screened regularly as a part of comprehensive geriatric assessments. Each year, the health care system loses billions of dollars due to falls and fractures in the geriatric population. Osteoporosis is common cause of fractures in both male and female older adults and it is preventable and under screened disorder [7]. It is estimated that one-third of older adults fall each year, and half of those individuals fall more than once a year, leading to including multiple hospitalizations, loss of function, fractures, institutionalization, and death [8]. The CDC developed STEADI due to worsening public health problem of falls in older adults [9]. Clinicians now can use the STEADI screening questionnaire to identify patients who are at risk for falls and offer effective interventions for fall prevention [10].
The purpose of this quality improvement project is to reduce the risk of falls and identify patients with undiagnosed depression using the STEADI fall screens and subsequently PHQ 9 depression screening test.
Study Methods
Using Plan-Do-Study-Act (PDSA) quality improvement methodology, a retrospective chart review was done from June 2017 until Nov 2018 (Figure 1). STEADI fall screens and PHQ-9 depression screening questionnaires of the Community- Dwelling elderly Population seen at the Geriatric Outpatient Clinic at the University of Toledo Medical Center (UTMC), were reviewed. All patients over the age of 65 seen at the geriatric clinic were included.
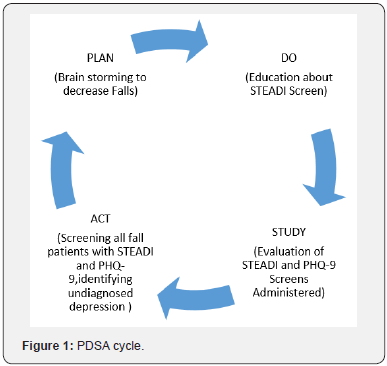
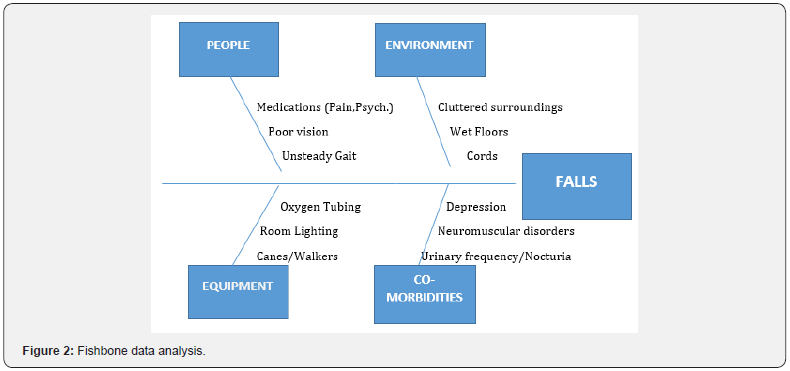
Plan: The geriatric clinical practitioners observed that many of the patients answered “yes” to the depression question in the STEADI Fall Screening questionnaire but were not screened for depression. They also noted that those with a formal diagnosis were not treated appropriately for the severity of depression. Interdisciplinary Team (IDT) consisting of physicians, pharmacy services, and clinical social worker used data analysis and fishbone diagrams (Figure 2) to identify areas of improvement.
Do: We created a presentation on STEADI Fall Screen and its different components to educate staff for active screening for depression in all geriatric patients answering “yes” to the depression screening and treatment questions in the STEADI Screen. Our geriatric team used monthly staff meetings and clinic days from August 2018 till October 2018 to educate and remind the providers including fellows, residents and medical students about the importance of STEADI fall screen and PHQ-9 screening in our fall patients.
Study: In November 2018, after our educational phase, we are currently monitoring our patients by screening everyone with a STEADI Fall screen and PHQ-9 screenings simultaneously. Primary outcomes involved a decrease in the number of falls. Secondary outcomes included identification of early depression and appropriate treatment of depression depending on the severity of symptoms.
Act: We will continue to monitor patients for falls and depression to achieve 90% screening goal for all patients in our geriatric clinic. We will continue to study the treatment of depression and prevention of falls in the next PDSA cycle.
Results
A total of 4,585 patients (1890 (41.1%) Males and 2695(58%) Females) over 65 years of age coming to the Geriatric outpatient clinic were studied (Figure 3). Out of the 4585 patients 3537 (77%) were white, 789 (17%) were African Americans, 69 (1.5%) were Hispanic, 41(0.9 %) Asians, 30 (0.6%) Middle Eastern and 13(0.3%) patients did not disclose their race. On reviewing STEADI fall screens of the total study population, 2709(59%) patients scored (0-3), 828(18%) scored (4-6) while 1048 (23%) scored >7 (High Fall Risk).
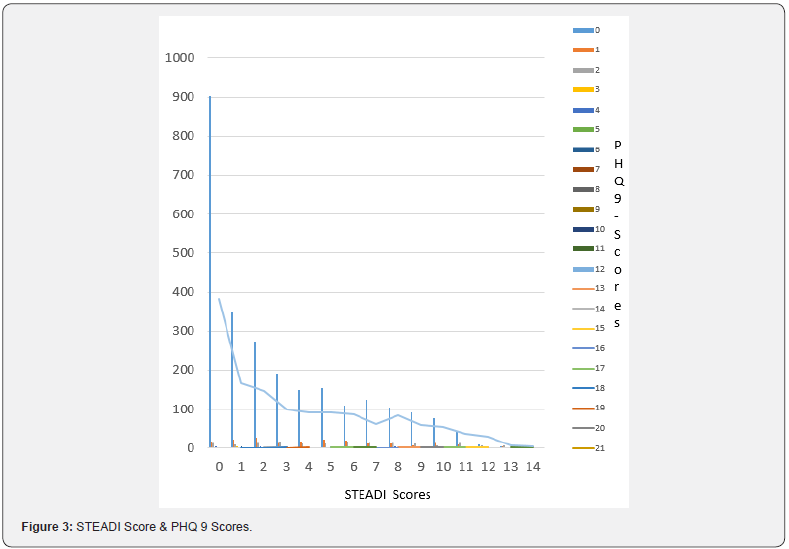
Depression screening with PHQ-9 was done in 3182(69%) patients while 1403(30.5%) patients were not screened for depression. The 3182 geriatric patients who were screened for depression with PHQ-9, 3016 patients had minimal depression (scoring 0-4), 77 had mild depression (scoring 5-9), 45 had moderate depression (scoring 10-14), 33 had Moderate to severe depression (scoring 15-19) and 13 patients had severe depression (scoring 20-27) on the PHQ-9.
There were 459 (10%) patients with a negative depression screen PHQ=0 but with a STEADI score >7. Most of the patients with moderate to severe and severe depression were whites (32) followed by African Americans (9).
Discussion
Many studies have examined the relationship between falls, depression and hospitalizations but few studies have explored the relationship between screening tools for falls and depression [11]. Our study examined STEADI fall screen questionnaire and its significance in screening undiagnosed depression in older adults. Our research helped us identify opportunities for improvement in our practice.
STEADI fall screen questionnaire gave us information about the functional status of our patients beyond just the fall risk; it helped us improve depression screening and subsequent treatment in the outpatient setting. Instead of focusing on only the final STEADI score, we looked specifically for the answers to the questions pertaining to depression. We found that out of the 4585 charts, only 69% of the patients had depression screenings performed.
By enhancing the depression screening for the elderly population, we have improved problems with polypharmacy with the help of pharmacy services in the clinic. Also, we have been able to use our psychology services to minimize medication use for depression and increased the utilization of cognitive behavioral therapy.
Prior studies demonstrated that depression is one of the major risk factors for falls, and other risk factors including multiple medications, ancillary walking devices, especially in institutionalized elderly with the neural system diseases. Fall prevention strategy should also include early identification and treating depression in older adults with poor medical conditions [12].
In the next PDSA cycle, we plan to continue to educate our staff and identify high risk patient populations. We will also evaluate the appropriateness of treatment of depression in our geriatric population, monitor for side effects and associated drug interactions with the help of pharmacy staff in our clinic.
Conclusion
By examining STEADI fall screen questionnaire and its significance in screening undiagnosed depression in older adults, we were able to identify opportunities for improvement in our practice. We found that STEADI fall screen questionnaire can give us information about the functional status of our patients beyond just the fall risk, including identifying patients with underlying undiagnosed depression.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php


No comments:
Post a Comment