Juniper Publishers- Open Access Journal of Case Studies
Intraductal Phyllodes Tumor in a 12-Year-Old Girl. Case Report and Literature Review
Authored by Catalina Vargas
Abstract
Breast masses in adolescent women and tumors with intraductal growth pattern are inusual. We report the case of a 12-year-old girl with a palpable breast tumor and discharge from the nipple, with a solid cystic mass in the ultrasound, resulting in a benign phyllodes tumor with intraductal growth on pathology, after surgical excision. We chose a conservative surgical behavior and close follow-up, in accordance with the few cases reported in the literature, given the unknown nature and uncertain prognosis of these tumors.
Keywords:Intraductal; Intracystic; Phyllodes, Fibroadenomatosis; Fibroadenoma
Abbreviations: PT: Phyllodes Tumor; RB: Right Breast; LB: Left Breast; UUQ: Union Upper Quadrants; UOQ: Upper Outer Quadrant; LOQ: Lower Outer Quadrant; RA: Retroareolar; FN: Fine Needle; CN: Core Needle
Introduction
Breast diseases are rare in adolescent women and most of them are benign. Breast tumors correspond mainly to fibroadenomas, phyllodes tumor (PT) and papillomas [1]. On the other hand, the intraductal growth pattern in fibroepithelial tumors is extremely rare, and its pathogenesis and prognostic implications commonly unknown. We present the case of a 12-year-old girl with a breast tumor whose histology is compatible with a benign PT with intraductal growth.
Case Report
A 12-year-old female patient without morbid or family history of relevance, with menarche at age 11, presents a palpable retroareolar mass in the left breast, which was associated with pain and serous secretion from the nipple 4 months ago. On physical examination, a tumor in the retroareolar region of the left breast of 3 cm in diameter is palpated and serohematic secretion is observed by ipsilateral nipple, suspicious axillary adenopathies were not palpated. It was studied with breast ultrasound that showed a left retroareolar lesion of complex structure and lobed appearance, with echogenic areas of irregular structure and areas of liquid content, 4,2 x 3,1 x 4,2cm. The color Doppler study showed little vascular flow in its periphery, concordant with an intracystic papillary lesion (Figures 1A & 1B). A complete surgical excision of the lesion was performed through a periareolar arciform incision, and the patient was discharged the same day of the intervention. The gross examination of the surgical specimen evidenced a solid-cystic, well-defined and capsulated ovoid tumor, 3,9 x 3,4 x 2,6cm (Figure 2A), and the microscopic examination showed a biphasic-fibroepithelial tumor, concordant with PT with pattern of intraductal growth, histological signs of benignity and negative surgical edges (Figures 2B & 2D). Follow-up was performed with postoperative control and at 6 months, both without clinical and imaging signs of recurrence.
Discussion
Fibroadenomas are the most common breast tumor in adolescent women, correspond to 60-90% [2] and are composed of epithelial elements and fibrous connective tissue [3]. PT are rare fibroepithelial lesions, corresponding to less than 1% of breast neoplasms, being particularly rare in girls and adolescents. They have stromal and epithelial elements, with a leaf-like architecture and a stromal component relatively larger than fibroadenomas. They have a broad spectrum of behavior, being classified as benign, borderline and malignant, according to the degree of stromal and atypia cellularity, mitotic count, stromal overgrowth and the compromise of their edges [4]. The papillomas are usually benign, consisting in intraductal stromal stem cells covered by a luminal layer of columnar epithelial cells and an outer layer of myoepithelial cells [5].

Breast tumors with intraductal growth are very rare and their pathogenesis is unclear. One hypothesis mentions that the growth of the periductal fibrous stroma can obstruct the lumen of the duct, causing intraductal fluid retention and dilation of the distal portion of the duct, causing the tumor to protrude into these dilated ducts [6]. Recently, intraductal lesions of benign histological appearance have been described, with overlapping characteristics of fibroadenoma, benign phyllodes tumor, papilloma and intraductal adenoma, finding intermediate characteristics that suggest a common or similar development [7].
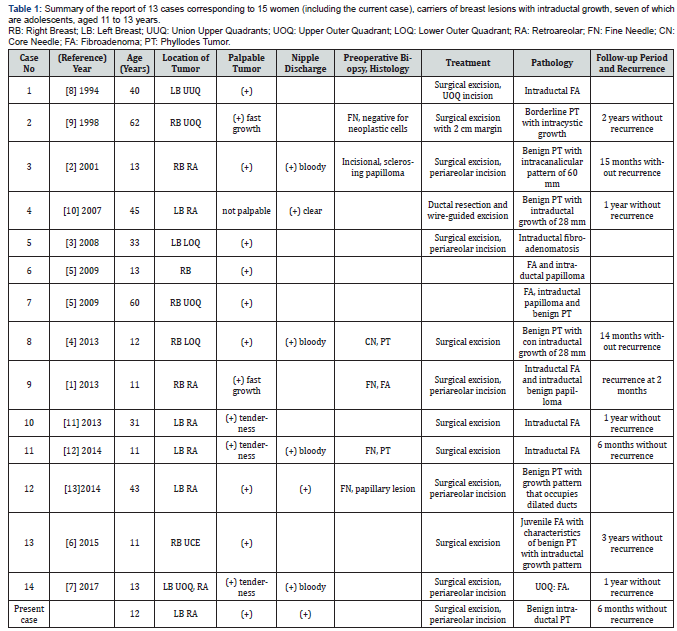
Reviewing the literature, we find 13 case reports (Table 1), corresponding to 14 women with breast lesions with intraductal growth, seven of which are adolescents, ages 11 to 13 years. The most frequent clinical presentation corresponds to a palpable mass (except in one patient) and serum discharge through the nipple (present in 6 cases). All patients underwent simple surgical excision, except one where resection with wide margins was contemplated. The histological study showed 5 lesions with mixed growth, identifying 9 fibroadenomas, 7 PT (six benign and one borderline) and 4 papillomas, all with intraductal growth.
The follow-up is described in 9 patients (between 6 months to 3 years), with only one early recurrence diagnosed on ultrasound performed two months after surgery, which was resected, informing a histology similar to the original lesion (benign PT).
The cases identified present several similarities to our patient, highlighting the significant proportion of cases described in adolescents. Although this infrequent pathology prevents an association with age, it seems interesting to inquire if the developing breast has any predisposition to develop tumors with intraductal growth. Similarly, the clinical presentation between cases is concordant, highlighting the retroareolar location and presence of discharge through the nipple as a background that can guide this type of lesions. In relation to the complementary study, it should include a breast ultrasound, and according to the findings, a percutaneous tumor biopsy may be recommended. It is suggested to maintain a conservative surgical behavior, especially in adolescent patients with still incomplete breast development and a predominantly benign pathology frequency, points that were considered and motivated the complete scission of the tumor without wide margins. Once the benign histology is confirmed, it is recommended to keep a close clinical and imaging follow-up, since despite the good behavior expected, there is a report of recurrence in a benign phyllodes tumor with intraductal growth.
The low incidence of breast disease in adolescents, added to with the unusual histopathological description of intraductal lesions, causes difficulties in differential diagnosis and uncertainty when deciding which is the best therapeutic strategy, due to the unknown etiology and uncertain biological potential of these tumors [1]. It has clinical implication to have a precise histological determination of lesions with these characteristics, and to base the hypothesis of the common development among known entities such as fibroadenoma, benign phyllodes tumor and papilloma, which have widely researched treatments and well-known prognoses. Assuming this theory, allows us to use similar behavior and consider conservative surgical options with complete scission of the lesion without requiring more aggressive resections to ensure free margins as is done with malignant tumors, maintaining a strict clinical and radiological follow-up, as long as the risk of recurrence and malignant transformation of these lesions based on the follow-up of the reported cases and the deeper study of the nature of these tumors [1,7].
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment