Juniper Publishers- Open Access Journal of Case Studies
Spontaneous Pneumomediastinum : Conundrum of Unusual Complication of Covid19 (A Case Report)
Authored by Ezzouine Hanane
Abstract
The symptoms of SARS-CoV-2 infection have been widely characterized in large studies, with fever, cough, and dyspnea being the most frequent. These same studies indicate that only 1-2% of patients developed pneumothorax, although it may occur as the disease progresses,its presentation is still infrequent, like pneumomediastinum. The mechanism is not fully elucidated, although it is probably because of rupture of the alveolar wall due to the increasing pressure difference between the alveolus and the pulmonary interstitium. Here we report a case of a 67 year old male who presented with a spontaneous pneumomediastinum in COVID-19 pneumonia, followed by a severe course of disease. We discuss the pathophysiological mechanisms underlying this association as well as its possible clinical implications as a marker of disease severity in COVID-19.
Keywords:COVID-19 ; SARS-CoV-2 ; Spontaneous pneumomediastinum ; Intensive care
Introduction
The coronavirus disease 2019 pandemic, COVID-19, has affected more than 200 countries with more than eight million cases confirmed as of June 1, 2020. Similar to severe acute respiratory syndrome in 2003 and Middle East respiratory syndrome in 2012, COVID-19 infection primarily causes life-threatening pneumonia, suggesting that the virus primarily targets the respiratory system and is spread through droplets of air and through contact. Chest computed tomography has become an important instrument to diagnose COVID -19, but it is also used for severity stratification and monitoring of disease. Here we present a case of spontaneous pneumomediastinum in COVID19 pneumonia, and discuss the possible mechanism underlying this association as well as clinical implications.
Case Report
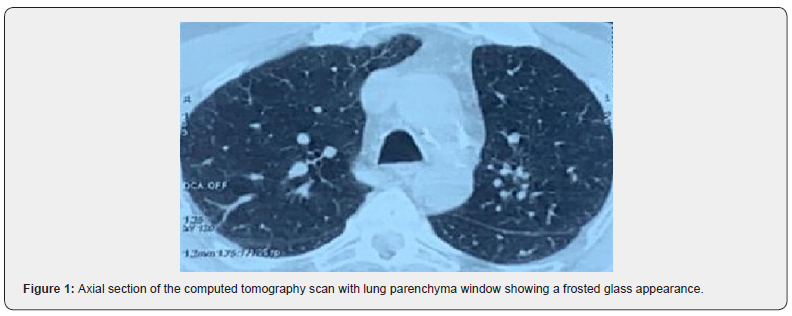
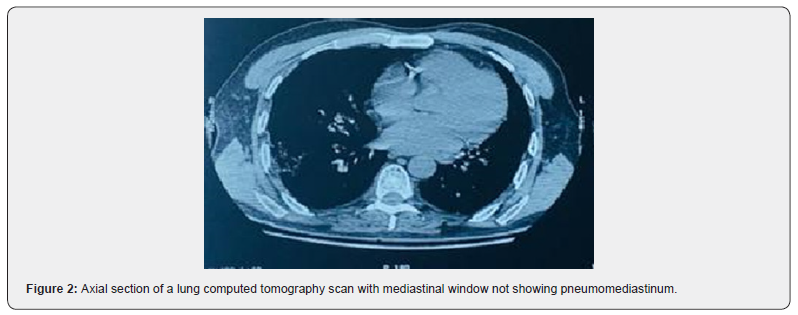
Patient aged 67years old, chronic smokerat 40 pack per year, with chronic obstructive pulmonary disease. The history of the disease goes back fifteen days ago with the onset of respiratory discomfort, dry cough, fever and flu syndrome. The patient was admitted first time to the emergency room where a thoracic scan was performed, which revealed a frosted glass appearance in favor of a viral attack (Figure 1 & 2) as well as art-PCR for SARS-COV-2 which came back positive. In front of the worsening from the symptomatology, the patient was transferred to intensive care unit.
On admission, the patient was conscious, his blood pressure was at 120/80mmHg and his heart rate was at 100beats/min. He suffered from hypoxemia, his pulse oxiymetry was at 70% in ambiant air which increased to 93% with high concentration of oxygen. He had dyspnea with respiratory frequency at 38 cycles per minute. His body temperature was at 37°C.
The Electrocardiogram showed regular sinus rhythm at 74bpm, fixed PR spaceat 0.16 seconds, thick QRS, QT measured at 320ms and QT corrected at 350ms without repolarization disorders.
The biological findings were as follows CRP at 55mg/L, hemoglobin at 17g/dl, leukocytes at 15410/μL, polynuclear neutrophils at 13950/μL, lymphocytes at 840/μL and platelets at 105000/μL. Urea at 10mmol/l, creatininemia at 70μmol/l, Natremia at 140mmol/l, kaliemia at 4.1mmol/l, fibrinogen at 2g/L, the prothrombin ratio at 100%, activated partial thromboplastin time at 30 seconds.
Arterial gas monitoring shows first time at ambiant air, pH at 7.34, PaCO2 at 52mmHg, PaO2 at 61.1mmHg, HCO3 at 25.5mEq/L with a PaO2/ FiO2 ratio at 119.8.
Transthoracic echocardiography noticed a moderate concentric left ventricular hypertrophy with an ejection fraction estimated at 55%, mitral profile with type of relaxation abnormality, no valve disease, good right ventricle and undilated inferior vena cava.
Therapeutic management included oxygenotherapy, the association hydroxychloroquine 200mg three times per day added to azithromycin 500mg the first day then 250mg per day and methylprednisolone at 80mg per day for 7 days, vitamine C 1 gramme per day and zinc 90mg per day and low molecular weight heparin enoxaparin 100UI/kg/ day.
The evolution was marked by a worsening of the respiratory symptoms, shortness of breath, cough and tachypnoea, without subcutaneous emphysema.
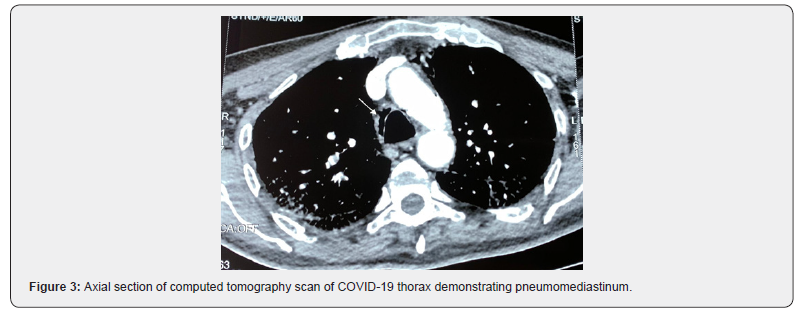
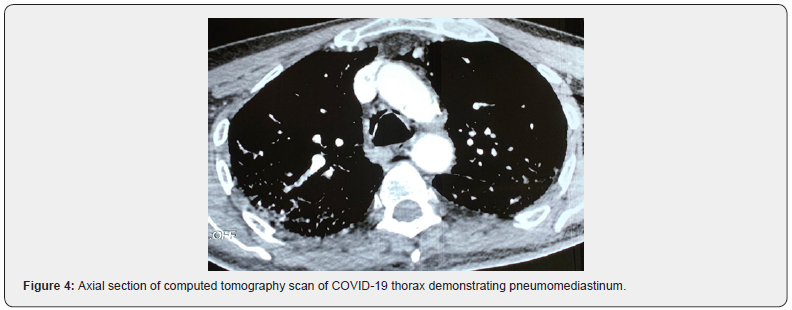
A chest computed tomography with contrast injection showed a diffuse interstitial pneumonia associated with pneumediastinum not pre-existing without pulmonary embolism (Figures 3 & 4). The patient needed to be intubated on the 5th day of hospitalization.
Discussion
The symptoms of SARS-CoV-2 infection have been widely described withthe most frequent signs, fever, cough, and dyspnea. However some complications are fewly reported as spontaneous pneumothorax 1-2%, and exceptionally spontaneous pneumomediastinum as the case we report [1,2].
Spontaneous pneumomediastinum is a rare complication of viral pneumonia. It has been described in severe acute respiratory syndrome (SARS) virus infections, influenza and bacterial pneumonia with rare strains. The causes of pneumomediastinum are varied. It is most often caused by increased airway pressures, secondary to mechanical ventilation or airway obstruction. However, other causes include a rise in intra-thoracic pressure such as from the Valsalva maneuver, strenuous activity, severe vomiting in diabetic keto-acidosis and anorexia nervosa, trauma to the thoracic cavity, oesophageal rupture, thoracic and head and neck surgery particularly with resultant tracheobronchial injury and alveolar injury due to underlying disease suchas infection and sarcoidosis [3]. Spontaneous pneumomediastinum associated with COVID -19 has occasionally been reported [4].
The pathophysiology of COVID-19 is purported to involve a cytokine storm in the airway that causes diffuse alveolar damage which added to the increase of intra-alveolar pressure, as seen in intentional Valsalva maneuver such as coughing, may lead to alveolar rupture [5]. Subsequently, this alveolar air circulates through the bronchovascular sheaths towards the mediastinum, following a negative pressure gradient. This pathophysiological mechanism is known as the Macklin effect [6].
Although spontaneous pneumomediastinum is generally considered a benign and self-limiting condition, its appearance in viral pneumonia may be of clinical significance as it has been previously suggested to be a potential indicator of disease severity. For instance, in SARS-COV-2 patients it was observed that the development of a spontaneous pneumomediastinum was associated with significantly higher rates of intubation and mortality [7] as was the case of our patient. Spontaneous pneumomediastinum is often self-limiting with no interventions required. However the tension pneumomediastinum can be lifethreatning and induce a severe cardio-pulmonary dysfunction [6].
This case highlights the emerging association of COVID-19 with spontaneous pneumomediastinum and the need to be alert to this complication in the evolution of the disease even in patients who had never received mechanical ventilation or positive airway pressure support.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment