Juniper Publishers- Open Access Journal of Case Studies
Use of Anticoagulants in a Von Willebrand Patient After Myocardial Infarction
Authored by Lesa Boone
Abstract
There has been great progress in the treatment and care of bleeding disorder patients. We have new factor products, new treatment modalities, and opportunities for collaborative care. These advances now allow patients to live a full life span. Along with these advances come the challenges of managing health alterations experienced in the adult and geriatric stages of life such as co-morbidities, alterations in self-care abilities, and decline in physical function. One of the greatest concerns include cardiac and vascular conditions. This case study outlines the experience of providing appropriate and effective coagulation services following myocardial infarction.
Keywords:Bleeding disorder; Anticoagulant therapy; Bypass surgery; Hemophilia treatment; Venipuncture
Case Study
Recently we had the opportunity to care for a Von Willebrand (VwD) patient who was placed on anticoagulant therapy. This patient was a 47-year-old female with type I Von Willebrand disease. Historically this patient had not required frequent bleeding disorder treatments other than for surgery or trauma. In 2018, the patient was a smoker who lived a reasonably sedentary life. She had hyperlipidemia and chronic back pain, both of which were being managed by her primary care provider. Her family history of significance included her father who had quadruple bypass surgery when he was 55 years of age.
One summer evening in 2019, the patient experienced chest pain and was taken to a local ER for evaluation of myocardial infarction. The patient was found to have an occlusion of one of her main coronary vessels requiring placement of a drug-eluding stent and initiation of dual anticoagulant therapy. The patient requested the emergency room staff call the hemophilia treatment center (HTC) for guidance however that communication did not occur.
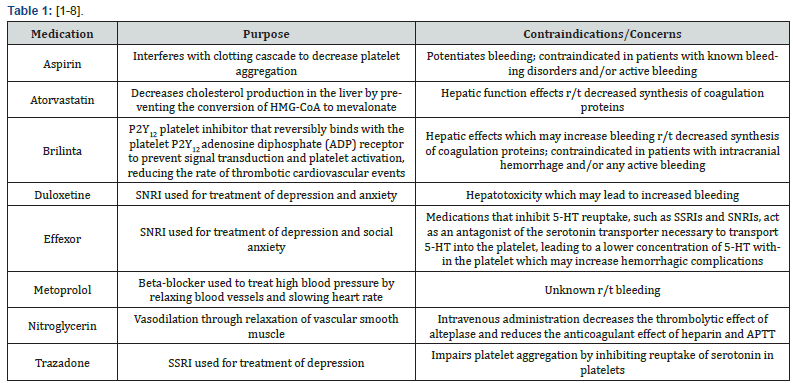
Six weeks later, the patient was scheduled for her yearly VwD appointment in the HTC where the team learned of her cardiac event. She also had challenges with anxiety at this time. During the appointment, the patient reported increased bleeding when brushing her teeth, increased bruising, and small soft tissue hematomas. The HTC team proceeded to gather data and began to outline a plan of care to manage this patient while on dual anticoagulant therapy for the next 12 months. The patient’s baseline VwD values were Factor VIII (42), Von Willebrand Activity (45), and Von Willebrand Antigen (58). Each of these labs were below the normal range. Her current medication profile included Table 1.
In an effort to collaborate regarding care, the HTC provider contacted the patient’s cardiologist who was unwilling to change anticoagulation therapy despite documented coagulopathy concerns and bleeding symptoms. Therefore, the HTC was obligated to try and balance the coagulation status of the patient in an effort to prevent any detrimental bleeding events. New labs were collected at the initial visit: PTT of 37.6, Factor VIII of 75, VW Activity of 41, and VW Antigen of 60. Platelet Function Assay revealed Collagen/Epi > 300, Collagen/ADP > 300 and von Willebrand multimers were within normal limits.
Based on current labs and presenting symptoms, the patient was started on VonVendi 2600 IU IV every 48-72 hours through a peripherally inserted central catheter (PICC) within 7 days of the HTC visit. A line was placed as the patient was not proficient in self-infusion and would require vascular access over the next year for factor administration. The HTC provided education and training to the patient and her husband in order to promote an adequate support system for the next year of bleeding disorder care. The patient was referred to a home care company who provided additional support for central line triage and maintenance.
The patient began with VonVendi administration 2-3x/week and lab evaluation weekly. Although labs were ordered weekly, labs were not always performed as requested, specimens were misplaced, and as time went along, the patient did not perform weekly lab draws as initially planned. See the Table 2 below for lab analysis Figure 1.
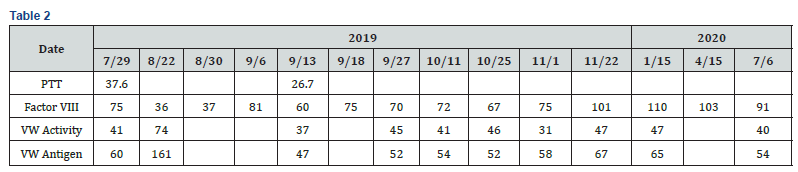
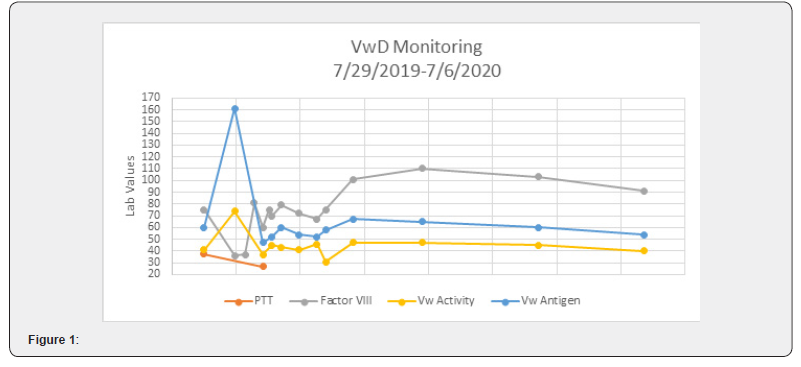
During the first six months, the patient was compliant with frequent lab analysis and evaluation. She reported that mucocutaneous bleeding events had basically resolved and her bruising had greatly diminished. Patient reported feeling well at follow up clinic visits and telehealth interactions. As she continued to do well, the frequency of her lab visits diminished. During October, the patient reported that she felt well and requested that her dosing regimen be decreased to 1-2 doses/week. A twice a week dosing regimen continued through January 2020 without difficulty.
During a follow up visit in January 2020, the patient requested that her PICC line be removed and that she begins to perform venipuncture to administer factor. The HTC collaborated with home health nursing to provide training for self-infusion and ongoing support for factor administration in the event the patient was unsuccessful with self-infusion. Patient received factor for 18 weeks via venipucture. During April 2020 visit, patient requested the VonVendi dosing regimen change to weekly infusion through June when her antiplatelet therapy would end. We encouraged ongoing use of product through the end of anticoagulant therapy and that if epistaxis, gum bleeding, or soft tissue hematomas returned, we would need to increase the frequency of factor dosing. Patient’s last clinic visit was 7/6/2020 which was day 393 since the patient’s initial cardiac event and day 364 since the start of VonVendi infusions. Patient reported no bleeding issues and no physical or psychosocial/emotional complaints or concerns during this final visit and VonVendi was discontinued. She continued to take low dose Aspirin, Atorvastatin, Duloxetine, and Venlafaxine. Patient returned to routine VwD care and management, where we educated and promoted awareness regarding bleeding concerns for another year as patient remained on low dose aspirin and continued to take duloxetine and venlafaxine both of which have bleeding as an adverse reaction.
Discussion/Implications
This patient was an opportunity to continue learning about how to collaboratively manage cardiac conditions in bleeding disorder patients, especially when anticoagulants are being used to manage the patient’s condition. There will continue to be more bleeding disorder patients who will be need comprehensive care, education, and oversight related to the use of anticoagulants.
This case has created interesting discussions for the HTC team and there are additional implications for practice related to this year-long clinical management effort:
i. Consider incorporating heart health education in clinical interactions. Teaching our younger populations about cardiac health, exercise, and nutrition can raise awareness and hopefully promote healthy life decisions and subsequently decrease risk for cardiac disease.
ii. Create more evidence to support the appropriate Vw levels for patients on anticoagulants. Very little evidence has been identified that provides support for maintaining specific Factor VIII levels or von Willebrand levels to prevent significant bleeding sequelae while on anticoagulants [9].
iii. Collaborate effectively with cardiologists and provide education about how placement of various types of stents impacts anticoagulant use in order to develop a coordinated plan for bleeding control.
iv. Polypharmacy continues to be an important consideration in the management of bleeding disorder patients. It is important to consider not only anticoagulant medications, but also the impact SSRIs and other medications have on platelets as a potential side effect that may further impede adequate hemostasis.
v. HTCs need to build a body of knowledge and share clinical experiences about management of these patients. Identification of more case examples can help promote development of guidance documents for care of bleeding disorder patients who develop cardiac conditions.
Gaining evidence in the effective management of patients on anticoagulants will continue to be an important consideration. As treatment for bleeding disorders improves, patients are living a normal life span, which can lend to other health alterations such as cardiac compromise. We hope case analyses, such as this, can lend to helpful information promoting comprehensive HTC care.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php





No comments:
Post a Comment