Juniper Publishers-Open Access Journal of Case Studies
A Rare Case of Metastatic Malignant Paraganglioma : Following with F-18 FDG PET/MRI
Authored by Bedriye Koyuncu Sokmen
Abstract
Paragangliomas are rare tumors arising from undifferentiated cells of the primitive neural crest. We present a 43-year-old male patient with a glomus tumor in the left carotid space and a retroperitoneal tumor with bone metastases, with invasion of the left renal vein in the left paraaortic area posterior to the third part of the duodenum. Serum epinephrine and norepinephrine levels were high. A CT-guided trucut biopsy was performed from this lesion, and histopathological examination and immunohistochemical analyzes concluded the diagnosis of retroperitoneal paraganglioma. The tumor was judged to be secretive and inoperable; therefore, it was decided to treat it with radiotherapy and systemic chemotherapy.
Keywords: Paragangliomas; Neuroendocrine tumors; Computed tomography; Magnetic resonance imaging; PET/MRI
Introduction
Paragangliomas (PGLs) are rare neuroendocrine tumors originating from the neural crest that originate from chromaffin sympathetic tissues or parasympathetic paraganglia and can occur in a wide localization from the skull base to the pelvic floor [1]. Retroperitoneal paragangliomas are rare tumors. As only a minority of cases secrete catecholamines, they are usually non-functional tumors [2]. About 10% of paragangliomas arise outside the adrenal gland. Few cases of metastatic retroperitoneal paragangliomas have been reported in the literature [3].
Precise localization of primary and metastatic lesions is important because of the presence of critical vascular and neural structures in the vicinity of the mass. It can change the management strategy from surgery to radiation, radionuclide therapy or observation.
PET/MRI imaging systems have proven to be comparable to PET/CT in oncological imaging, and the use of MRI instead of the CT component has the theoretical advantages of lower ionizing radiation exposure, as well as improved soft tissue contrast and local tumor elaboration [4].
In this article, F-18 FDG PET/MRI findings and treatment response of a case of secretory retroperitoneal metastatic paraganglioma treated with radiotherapy and systemic chemotherapy are presented.
Case Presentation
Here, we present a rare case of retroperitoneal paraganglioma with bone metastases in a 43-year-old male patient.
The patient with a diagnosis of left glomus tumor known for 10 years was admitted to our hospital with the development of hypertension attacks. The blood pressure values were found to be 220/110mmHg in the mean measurements. In the clinical examination, our patient had a complaint of pain in the lumbar region.The patient had no smoking history or family history of paraganglioma or other neuroendocrine tumor. In the laboratory tests of the case; Urine normetanephrine value was 3358 (68-444) microgram, Vanillyl mandelic acid (VMA) was 17.1 (0-8), CrgA value was 451ng/ml and it was found above normal measurements. Urinary metanephrine value was within the normal range. Another blood tests, including liver and renal biochemistry were normal.
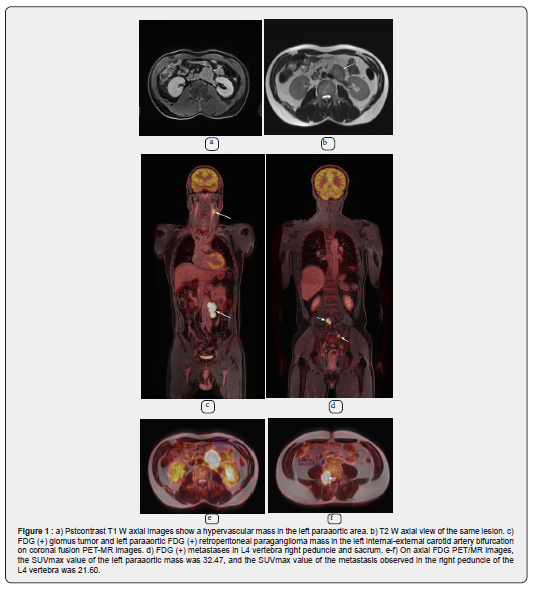
On PET MRI performed in January 2021, a 2x2.5cm FDG (+) mass from a glomus tumor was observed at the level of the left internal-external carotid artery bifurcation. (suvmax : 6.8) A mass lesion of approximately 3x5.5x7.5cm in size with irregular lobulated contours with FDG uptake (SUVmax: 32.47) and evaluated in favor of hypervascular retroperitoneal paraganglioma was observed in the left paraaortic area inferior to the third part of the duodenum. The defined mass seemed to invade the posterior adjacent left renal vein and the opening of the renal vein to the inferior vena cava, and surrounded the left renal artery more than 180°.
Metastatic lesions were observed in all vertebrae with FDG (+) 3.5cm in diameter, the largest of which was located on the right peduncle of the L4 vertebra (SUVmax 21.60). In addition, multiple FDG (+) bone metastases were observed in the manibrium sterni, on the right lower ribs, and bilaterally proximal to the femur (Figure 1).
A percutaneous biopsy of the L4 vertebra under CT guidance confirmed that the lesion was a paraganglioma metastasis.The patient was diagnosed with metastatic paraganglioma and underwent palliative chemotherapy.
Radiotherapy was applied to the metastases at the level of L4 vertebra with 35Gy and for the mass in the paraaortic area 45Gy. Simultaneous 12 cycles of systemic chemotherapy were also given. In chemotherapy, cyclophosphamide, vincristine and dacarbazine (CVD) were applied. Zoledronic acid was also given. Our patient received radiotherapy between January 8 and February 11. At the end of radiotherapy, our patient's blood pressure was within normal limits. (125/80mmHg)
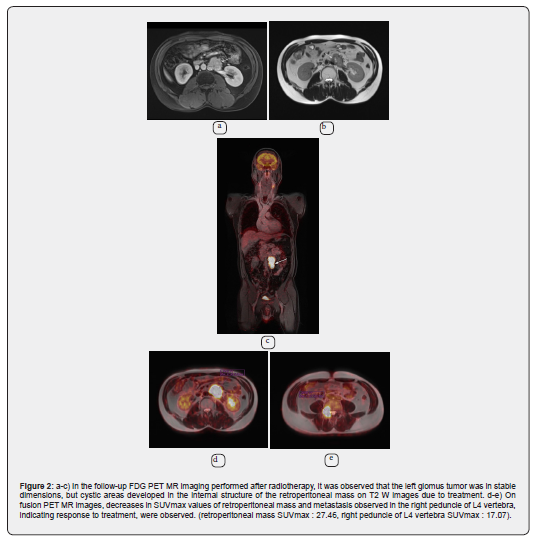
In the control PET MRI examination of the patient, which was performed in August 2021, the mass showing significant FDG uptake (SUVmax 27.46) in the retroperitoneum in the left paraaortic area, although there is no significant difference in size, shows metabolic minimal regression. In addition, there was metabolic regression (SUVmax 17.07) in the metastasis observed in the L4 vertebra. Mass lesion consistent with paraganglioma observed at the level of the left internal-external carotid artery bifurcation were stable (Figure 2).
Discussion
Paraganglioma is a rare tumor that usually occurs in the 3rd to 4th decades. 40% of paragangliomas produce high catecholamine levels, resulting in symptoms such as headache, palpitations, profuse sweating, and elevated urinary metanephrine or vanillylmandelic acid levels. The most common site of involvement for paraganglioma in the retroperitoneum is the organs of Zuckerkandl located anterior to the aorta at the origin of the inferior mesenteric artery [5].
Paragangliomas frequently occur with recurrence or metastasis, as 30% to 40% are hereditary and the other 15-20% carry somatic mutations in one of the more than 20 well-characterized PGL susceptibility genes [1].
Computed tomography (CT) and magnetic resonance imaging (MRI) are effective non-invasive imaging modalities for the detection and evaluation of paragangliomas. MRI has advantages over CT in better soft tissue contrast, higher intrinsic flow sensitivity, and non-ionizer [8]. Magnetic resonance imaging has proven superior to other imaging techniques in demonstrating a more accurate assessment of lesion margins and invasion of adjacent structures [6].
As it is known, Paragangliomas are hypervascular tumors with imaging features of soft tissue mass with intense contrast enhancement and “salt and pepper” appearance on MRI in conventional spin-echo sequences [7].
Diffusion-weighted imaging and ADC value measurement, which are functional imaging methods taken simultaneously in PET-MRI, are used as diagnostic or differential diagnosis tools in oncology [9].
Recently, [68Ga]-DOTATATE PET/CT has emerged as a more sensitive modality for identifying occult PGLs and metastasis by targeting somatostatin receptor 2 (SSTR2) overexpression at PGLs with greater affinity than other somatostatin receptor analogues. A new modality, PET/MR imaging systems have proven to be comparable to PET/CT in oncological imaging. The use of MRI instead of the CT component has the theoretical advantages of lower exposure to ionizing radiation, as well as improved soft tissue contrast and identification of the local tumor and surrounding structures. Some case studies showed much greater soft tissue contrast with [68Ga]-DOTATATE PET/MR compared to PET/CT in PGL patients, allowing for more accurate tumor identification resulting in changes in preoperative planning [10-12]. The prospective analysis of 8 PGL patients with [18F]-FDG PET/CT and [18F]-FDOPA PET/CT and subsequent PET/MR showed that PET/MR was superior for HNPGL, abdominopelvic PGL, and liver metastasis while equivalent to PET/CT for bone metastasis [13].
In the patient presented here, PET-MRI findings are more valuable than PET-CT in cases where the MR component is superior to CT in the detailed evaluation of the soft tissue component in the relationship of retroperitoneal paraganglioma with vascular structures, and in the detailed evaluation of the soft tissue component in bone metastasis.
Conclusion
Hybrid imaging PET/MRI examination is important in the identification of primary neoplasm as well as in the detection of distant metastases in a single session. Combined multi-parametric imaging improves patient comfort and is well suited for examining patients with hereditary syndromes and paragangliomas, especially in the pediatric population, given the lower radiation exposure compared to PET/CT as a replacement for the CT component.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php


No comments:
Post a Comment