Juniper Publishers-Open Access Journal of Case Studies
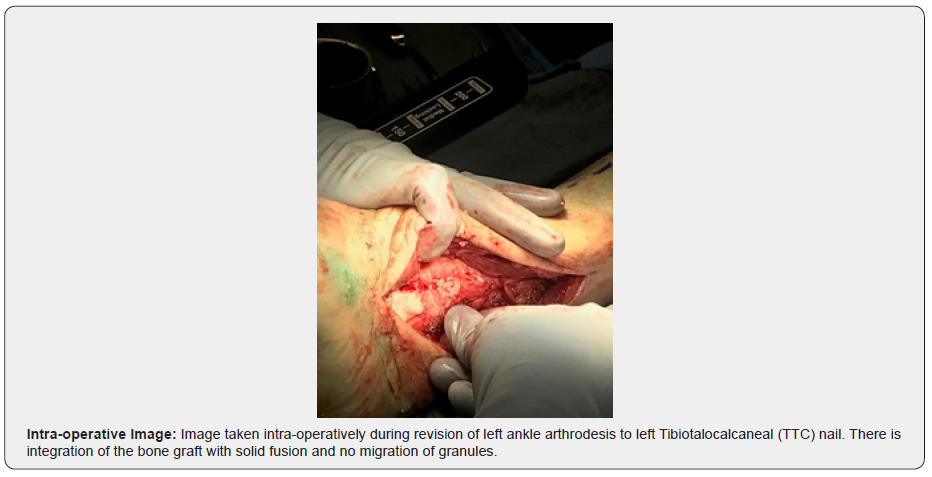
Clinical, Radiographic, and Histologic Outcomes of Ankle Arthrodesis in a Diabetic Patient using a Biphasic Calcium Phosphate Bone Graft with a Novel Submicron Needle-shaped Surface Topography
Authored by Thomas Fusco
Abstract
Patients with diabetes mellitus who sustain ankle fractures are at increased risk of complications including non-union, malunion, wound dehiscence, soft tissue infection, osteomyelitis, deterioration to Charcot arthropathy, and amputation [1-3]. Multiple publications have evaluated treatment options for diabetic patients with ankle fractures; management options include non-surgical treatment and immobilization, open reduction internal fixation, arthrodesis of the tibiotalar joint, arthrodesis of the tibiotalocalcaneal joints, external fixation, and amputation [4-7]. It is important to identify an effective bone graft for these cases, as well as to understand the science behind the bone graft selected. In recent years, the study of osteoimmunology has confirmed the reciprocal interaction of bone forming mesenchymal stem cells and immune cells on bone growth. This report describes an adult female patient with a late presenting ankle fracture dislocation, initially treated with ankle arthrodesis using a novel bone graft with submicron needle-shaped surface topography. The patient developed Charcot arthropathy and was revised to a tibiotalocalcaneal (TTC) nail. During revision, a biopsy was taken of a solidly fused segment and sent for histology. Radiographic, clinical, and histological data were tracked and showed solid fusion at 6 weeks radiographically, which was confirmed via histology and surgical exploration at 12 weeks, indicating notable results in this challenging arthrodesis case using a novel bone graft with submicron needle-shaped surface topography.
Keywords: Charcot arthropathy; Diabetic ankle fracture; Diabetic ankle arthrodesis; Osteoimmunology, Mesenchymal stem cells; Surface topography
Introduction
Patients with diabetes mellitus who sustain ankle fractures are at increased risk of complications including non-union, malunion, wound dehiscence, soft tissue infection, osteomyelitis, deterioration to Charcot arthropathy, and amputation [1-3]. There is no gold standard for treatment, as the success of both bony and soft tissue healing depends on factors such as fracture pattern, patient co-morbidities, hemoglobin A1c, the presence of neuropathy, the ability of the patient to remain non-weight bearing, and others [3]. Multiple publications have evaluated treatment options for diabetic patients with ankle fractures; management options include non-surgical treatment and immobilization, open reduction internal fixation, arthrodesis of the tibiotalar joint, arthrodesis of the tibiotalocalcaneal joints, external fixation, or amputation [4-7]. In 2021, a meta-analysis of open ankle arthrodesis reported an overall complication rate of 14% for this procedure [8]. In diabetic ankle fractures the reported complication rate is much higher, with one review reporting a complication rate of 47% [9]. One important challenge of arthrodesis in diabetic patients is identifying the most scientifically advanced bone graft for the procedure [10]. Synthetic calcium phosphate bone grafts closely resemble human cancellous bone, have an exceptional safety profile, and have proven to be a cost-effective alternative to autograft [11-13].
In response to tissue trauma or surgery, the immune system reacts by upregulating pro-inflammatory macrophages, also known as the macrophage M1 phenotype. If M1 macrophages are chronically activated a fibrotic healing response is initiated, ultimately leading to a non-union. Conversely, if the macrophage M2 phenotype is activated a pro-healing response is initiated, upregulating mesenchymal stem cells and promoting the formation of bone rather than scar tissue [14]. Utilizing a biphasic calcium phosphate (BCP) bone graft with needle-shaped submicron surface features (BCP<µm) polarizes naïve monocytes to the pro-healing M2 phenotype. In preclinical studies, this BCP<µm has been shown to promote bone formation even in soft tissue, without the need for added cells or growth factors [15]. This novel BCP<µm bone graft mimics the structure of cancellous bone, with bone formation taking place throughout the bone graft leading to a solid, uniform fusion that has been demonstrated in clinically relevant animal models [16,17].
This case describes an adult female patient with a late presenting ankle fracture subluxation, initially treated with ankle arthrodesis using a novel bone graft with submicron surface topography. The patient developed Charcot arthropathy and was revised to a tibiotalocalcaneal (TTC) nail. During revision, a biopsy was taken of a solidly fused segment and sent for histology. Radiographic, clinical, and histological data were followed for 24 weeks from initial surgery and 12 weeks from revision surgery.
Case
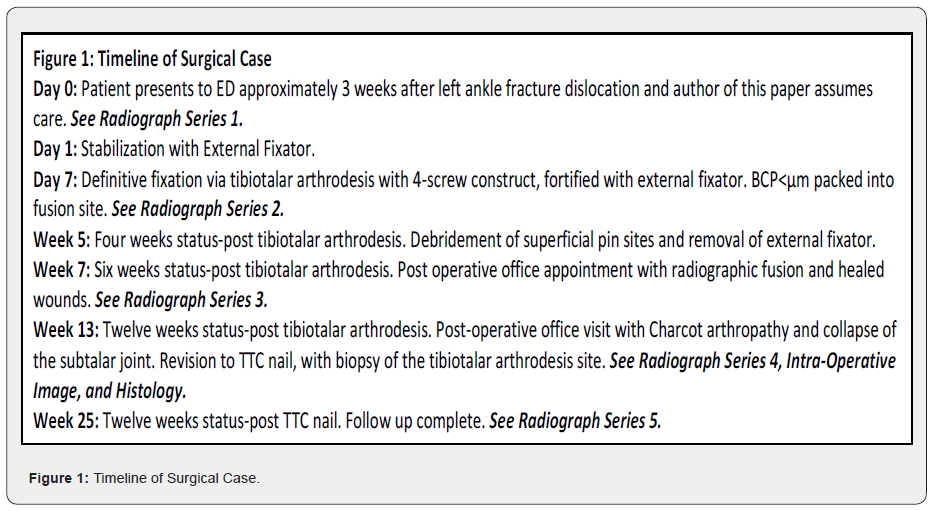
The patient is a 73-year-old female who presented to the emergency department three weeks status-post left ankle injury. The patient reported that three weeks prior she sustained a left ankle injury and went to the emergency department where she was diagnosed with an ankle fracture dislocation and underwent closed reduction. She was discharged for outpatient follow up at that time. Upon outpatient follow up, the patient reported that radiographs were obtained showing loss of reduction and repeat dislocation. She stated that she returned to the emergency department where she was re-reduced and splinted. Again, the reduction did not hold, and she returned to the emergency department. At this time, the author of this paper became involved. Radiographs from the emergency department on that day revealed a trimalleolar ankle fracture with subluxation See Radiograph Series 1.The patient’s past medical history included diabetes mellitus type II with neuropathy, peripheral artery disease, hypertension, hypothyroidism, hyperlipidemia, coronary artery disease, gastroesophageal reflux disease, and depression. On admission, her hemoglobin A1c was 9.1, and her body mass index was 36.9kg/m2. She denied the use of tobacco. For graphic representation of the surgical and post-operative timeline, see Figure 1.
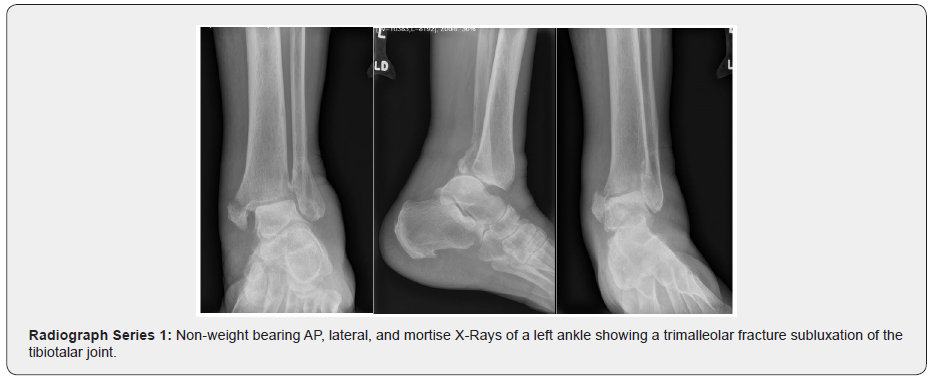
The patient was immediately admitted from the emergency department and scheduled for closed reduction and external fixator placement in the operating room. This procedure was performed uneventfully the following day. The patient was discharged home, planning to return to the operating room one week later for definitive fixation. At the time of definitive fixation, the external fixator was removed, and a tibiotalar arthrodesis was performed using a four-screw construct. This was fortified with placement of a new external fixator. During this procedure, a novel BCP bone graft with a needle-shaped submicron surface (BCP<µm)was used to pack the arthrodesis site. This surgery was uneventful, and the patient was discharged home as expected with instructions to remain non-weight bearing on the left lower extremity. See Radiograph Series 2.
Four weeks after definitive surgery, the patient presented to her post-operative appointment with concern for an infected external fixator pin. The decision was made to bring the patient back to the operating room for external fixation removal and thorough debridement. At that time the pin sites were cleaned and debrided, and questionable bone was explored with cultures sent to pathology. Clinically, the bone did not appear osteomyelitic, which was confirmed with multiple negative bone cultures. The patient was prescribed a full course of oral antibiotics.
Two weeks after removal of the infected external fixator, the patient returned for her six-week post-operative appointment. At that time, she was doing well. Her wounds were clean, dry, and intact, her edema was improving, and her radiographs showed a healing fusion site with hardware in good position without loosening or lucency around the screws Radiograph Series 3.
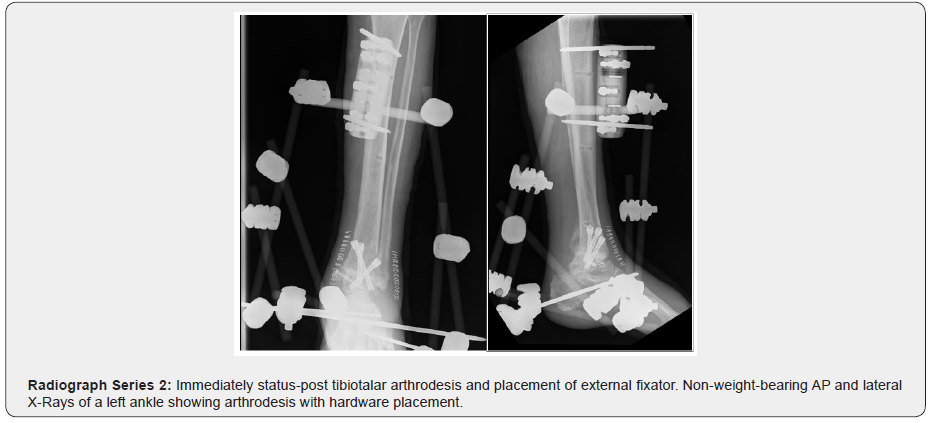
Three months status-post her definitive surgery, the patient returned for follow-up. Radiographs were obtained, which showed interval deterioration of her hindfoot with Charcot arthropathy collapse See Radiograph Series 4.A thorough discussion was held with the patient, and ultimately the decision was made to revise the tibiotalar arthrodesis to a TTC nail. During this procedure, the arthrodesis site was explored, and the novel BCP bone graft had integrated well into the fusion site with solid appearing bone and no migration of the granules. Biopsy of the fused segment was obtained and sent for histology See Intra-Operative Image.
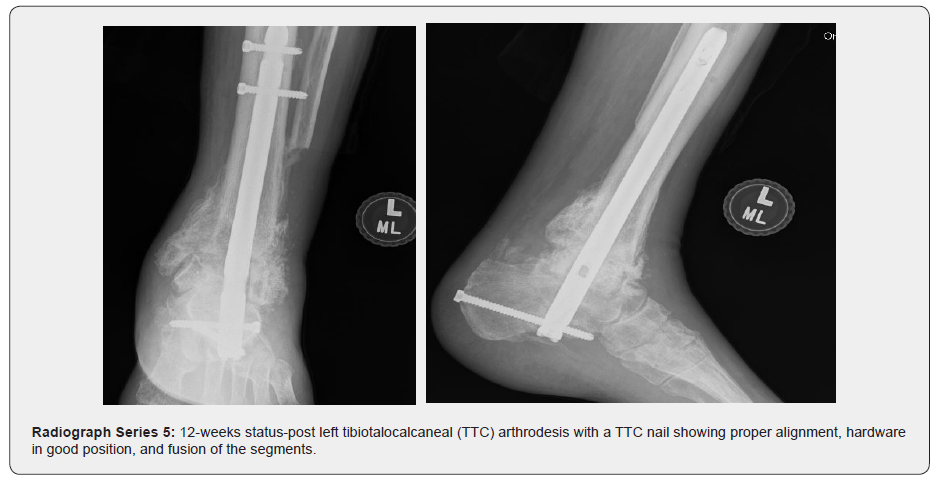
Following the TTC nail, the patient had an uncomplicated post-operative course. At her 12-week post-operative office visit she had no complaints, and her radiographs showed a well-aligned healing arthrodesis. The patient was cleared to begin weight bearing. Shortly thereafter, the patient moved to another state and was lost to follow up See Radiograph Series 5.


Biopsy Results
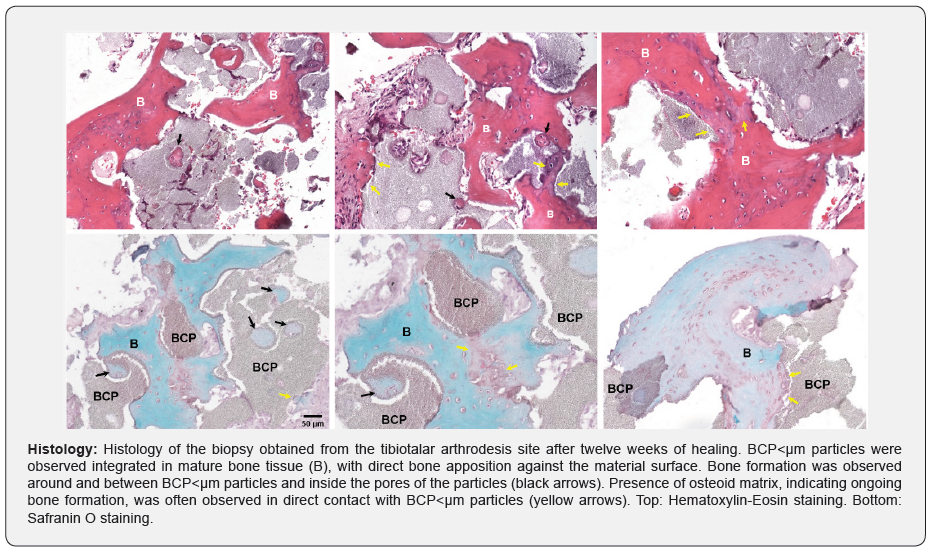
The biopsy obtained from the revision surgery at the tibiotalar arthrodesis site twelve weeks post-operatively was processed for routine bone tissue histology with hematoxylin-eosin and Safranin O stains. The biopsy showed mature bone tissue with integration of the BCP<µm bone graft. Bone was observed in direct apposition with the BCP<µm particles, growing around and between the material and inside its pores. Bone tissue around the material had a normal phenotype, including woven and lamellar structure, the presence of blood vessels, and cells such as osteoblasts, osteoclasts, and osteocytes residing in lacunae. Ongoing new bone formation, as characterized by presence of osteoid matrix, was commonly observed directly against the surface of the BCP<µm particles or inside their pores. No adverse reactions to the BCP<µm bone graft were observed See Histology.
Discussion
Ankle arthrodesis in Charcot arthropathy is known to lead to increased complications such as non-union, malunion, infection, and amputation [2]. Successful fusion depends on a variety of factors including patient age and co-morbidities, arthrodesis technique and implants chosen, and bone graft selected [3]. This case exhibits the benefits associated with the use of a biphasic calcium phosphate bone graft with submicron needle-shaped surface topography in achieving a reliable and solid fusion.
The patient, an elderly female with uncontrolled type II diabetes mellitus and Charcot arthropathy, is a difficult clinical scenario with a successful fusion outcome using BCP<µm bone graft. The patient had radiographic fusion via X-Ray at six weeks post-operatively from the index procedure. Additionally, due to the unforeseen complication of Charcot arthropathy at the joint below the fusion site, the surgeon was able to obtain histology from the original fusion site, which showed a significant amount of mature lamellar bone at only twelve weeks after the initial fusion with BCP<µm. The literature on specific bone grafts in ankle and hindfoot arthrodesis is limited; however, one large, prospective, randomized multi-center study evaluating rhPDGF-BB/β-TCP bone graft reported fusion outcomes of 61.2% as determined by Computed Tomography (CT) at six months post-operatively [18]. In contrast, this case was able to report fusion confirmed by X-Ray six weeks post-operatively, as well as by second look surgery and histology at twelve weeks post-operatively.
The case also highlights a successful fusion outcome in a procedure known to be technically difficult and fraught with risks such as infection and non-union. Recent literature reports high complication rates in both diabetic ankle fractures and TTC nails, with one review of diabetic ankle fractures reporting an overall complication rate of 47%, and another retrospective review reporting a non-union rate of 22.8% after subtalar arthrodesis via TTC nail [9,19].
In this case, the fusion was confirmed via multiple methods: clinically, radiologically, histologically, and via the gold standard for fusion assessment: surgical exploration [20]. Remarkably, this case demonstrated fusion via X-Ray at six weeks post-operatively, as well as mature lamellar bone formation via surgical exploration and histology at twelve weeks post-operatively. This report demonstrates that BCP<µm bone graft with needle-shaped submicron surface topography is an effective bone graft for use in complicated extremity arthrodesis procedures.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/manuscript-guidelines.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php



No comments:
Post a Comment